An innovative type of ultrasound scan that can detect cancer tissue left behind after a brain tumor is removed could improve the outcome from operations and reduce the risk of relapse, according to a new study published in the journal Frontiers in Oncology.
The technique, called shear wave elastography (SWE), could be used during brain surgery to detect residual cancerous tissue, allowing surgeons to remove as much as possible. The research team led by The Institute of Cancer Research and the National Hospital for Neurology and Neurosurgery in London said it has the potential to reduce the risk of patient relapse by cutting the chances that a tumor will grow back. According to them, it is also much faster and more affordable than the widely used MRI scans.
The team compared, in a sample of 26 patients, three different techniques to detect tumor tissue during surgery: shear wave scans, a standard 2D ultrasound, and a surgeon’s opinion. The researchers performed shear wave scans and 2D ultrasounds during the operation—before, during and after tumor removal. They also asked surgeons to identify potentially cancerous tissue before providing them with scan findings. The team then compared all techniques with gold-standard MRI scans after surgery.
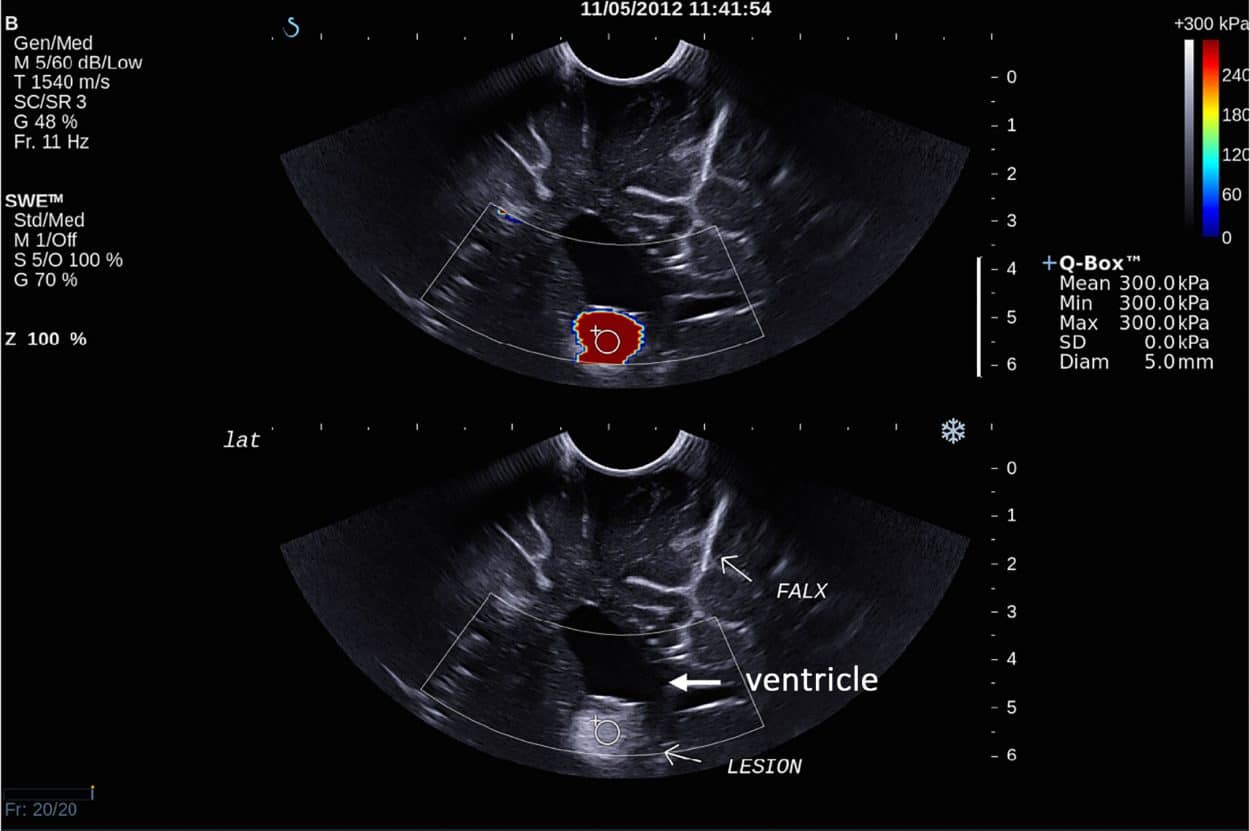
They found that shear wave elastography was more sensitive in detecting residual tumor tissue than a standard ultrasound or the surgeon alone. The new scanning technique detected tumor tissue with 94 percent sensitivity compared to 73 percent for standard ultrasound and 36 percent for the surgeon. This means that when there was residual tumor tissue, shear wave scans were 2.5 times better than the surgeon at detecting it.
The research was conducted in collaboration with clinicians from The Royal London Hospital and University Hospital Southampton in the UK. Study leader Professor Jeffrey Bamber, Professor in Physics Applied to Medicine at The Institute of Cancer Research, said:
“Ensuring all of a brain tumor is removed without damaging healthy tissue is a major challenge in brain surgery. Using this new type of scan, surgeons could greatly increase confidence that no cancerous tissue is going to be left behind after surgery. We have shown for the first time that this new tool is better than either a standard 2D ultrasound or a surgeon’s judgment on its own, and has the potential to supplement a surgeon’s opinion as a means of improving outcomes from operations.”
Shear wave elastography measures tissues’ stiffness and stretchiness. Vibrations or “shear waves” are created and detected as they move through tissue—moving faster through stiffer tissue. Brain tumors tend, on average, to be stiffer than normal brain tissue and the technique works by mapping suspicious areas of particular stiffness, which can then be examined and removed during surgery.
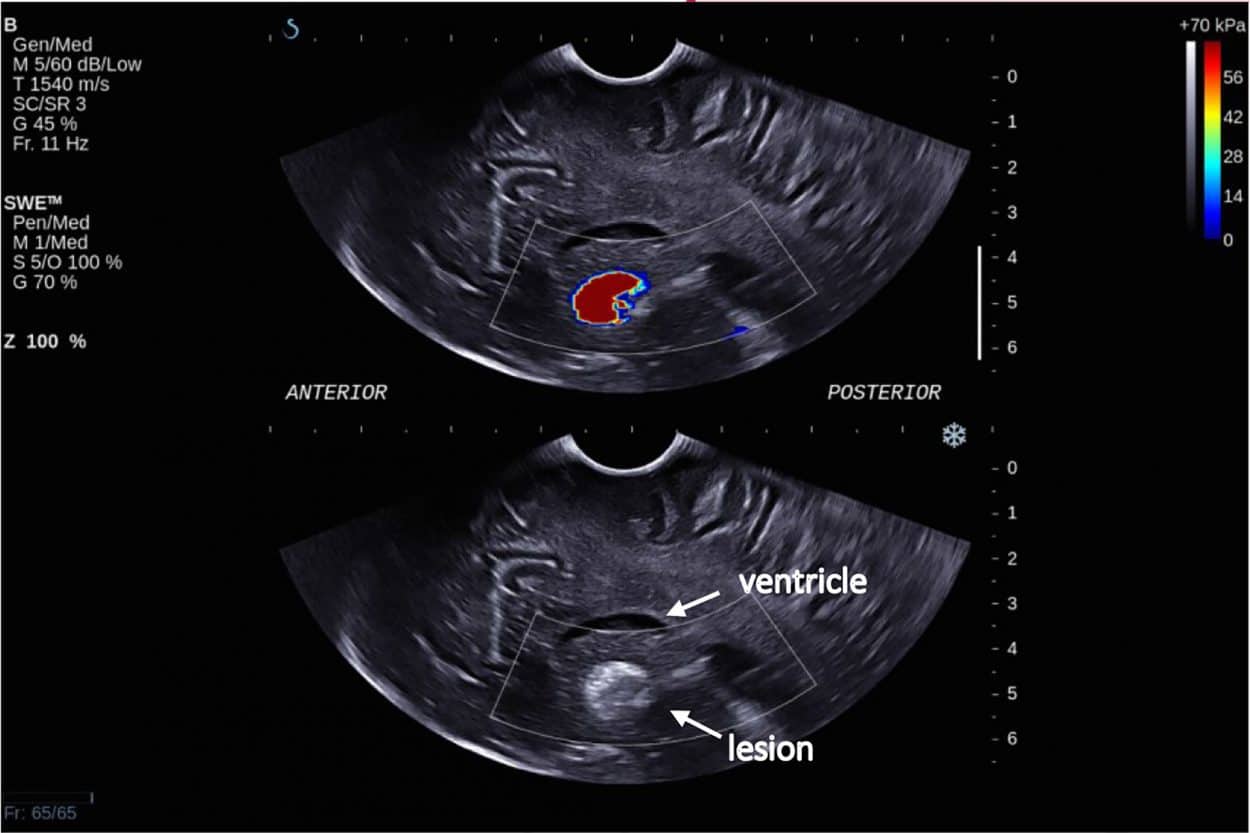
Patient outcomes from brain tumor surgery are known to be better when as much of the tumor as possible is removed. In order to make sure that none of the resectable tumor is left behind, neurosurgeons use tools to guide them during surgery. MRI scans are the most accurate, but are costly and not normally available in operating theaters. Shear wave scans were shown to be as good as post-surgery MRIs at detecting tumor tissue that had been left behind, making them a cheaper, faster and more feasible alternative.
Further Studies
The study is the first to demonstrate the potential of shear wave elastography as a neurosurgical tool to confirm during surgery the completeness of tumor removal. Further studies are now needed before the technique can become standard practice. Professor Kevin Harrington, head of the division of radiotherapy and imaging at The Institute of Cancer Research, said:
“Imaging plays a crucial role in many aspects of cancer treatment, in providing valuable information about tumors and ensuring doctors don’t have to make decisions blind. This new study has shown for the first time that a particular type of ultrasound scan could provide real-time guidance to brain surgeons during operations as they choose which tissue to remove. It’s an exciting area of research which has the potential to improve outcomes for patients by ensuring surgeons take out the entire tumor while minimizing damage to the healthy brain.”
Neil Dorward, Consultant Neurosurgeon and co-researcher at the National Hospital for Neurology and Neurosurgery, said:
“This technique provides a very practical means of detecting areas of potentially removable tumor that are not readily visible to the operating surgeon. The surgeon must use his or her experience to decide whether the area of abnormality should be resected. This has the potential to substantially improve the outcome of such operations.”