Medisanté has created a cloud-based infrastructure that specializes in transmitting medical data from connected devices in the home directly to a hospital doctor’s screen, effectively eliminating the need to go through a consumer’s smartphone. The Swiss company has just announced a partnership with the German manufacturer of electrical appliances Beurer, which should help it scale up in terms of logistics and device financing. This expansion is part of the remote monitoring reimbursement policies that are emerging throughout Europe following the Covid-19 pandemic. We spoke with Gilles Lunzenfichter, the CEO and co-founder of Medisanté.
MedicalExpo e-magazine: What is the advantage of your cloud?
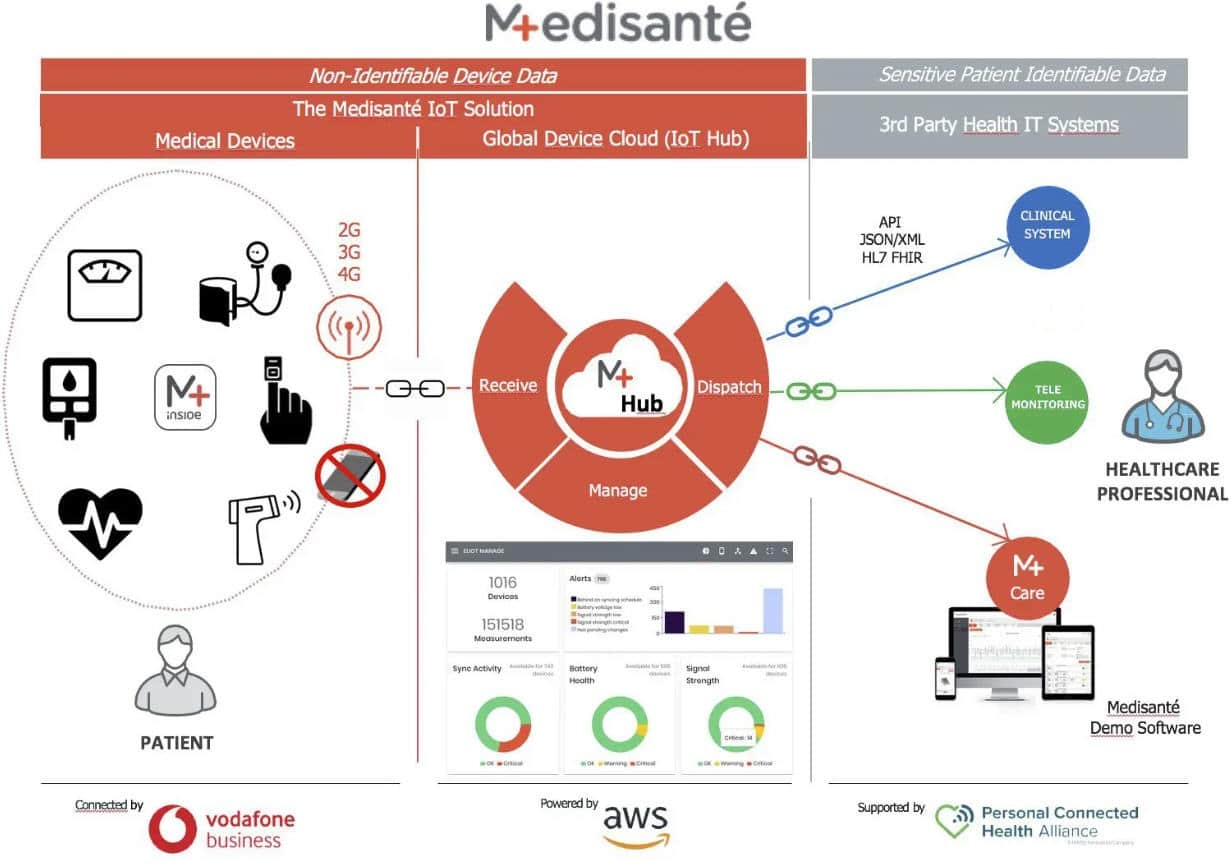
Gilles Lunzenfichter: The advantage is that all the patient has to do is take the measurement with the device he or she received from the hospital that chose to do remote monitoring, and the collected data is sent directly to that hospital via our cloud.
Today, it is often accepted that a person who needs telemonitoring must have a smartphone, be able to use it, download applications, remember passwords, etc. But for seniors this is not always easy. During the Covid-19 pandemic, it was said that we had to protect the most fragile, but the most fragile people were often elderly people who did not have a smartphone, or if they did, they did not necessarily know how to use it well.

So today there is a new generation of devices coming out that connect directly to a doctor’s screen. And to make this connectivity and interoperability between a device and the doctor’s screen possible, you have to get around each manufacturer’s software and go through a cloud infrastructure like ours.
So how does it work in practice?
Gilles Lunzenfichter: If, for example, the Timone hospital in Marseille wants to extract data from its patient Mr. Martin as part of a remote patient monitoring program, they will give Mr. Martin a device. This device could be a scale, a thermometer, a blood pressure monitor, an oximeter, a multimeter or an ECG monitor.
There are two possibilities: either the hospital provides these devices equipped with a sim card, or it provides a cellular gateway (a kind of telecom box at home) with a sim card inside and three bluetooth devices connected around it that automatically self-operate.



At home, Mr. Martin connects the gateway with a power cable, then, for example, measures his blood pressure with the blood pressure monitor provided. It’s very simple, he doesn’t need to configure anything, make any manual adjustments or have any technical or digital skills and he doesn’t have to be equipped with a smartphone or internet at home.
Once the measurement is taken, the data goes through the gateway, the gateway goes through our cloud, and our cloud sends the data to the hospital’s IT system which assigned the gateway and the devices to the patient in the remote monitoring program in the first place.
So, if Mr. Martin’s device is number 33 for example, the only place where our cloud can send data from device 33 will be to the Timone hospital in Marseille where Mr. Martin was assigned this device. The patient can be anywhere in the world, the doctor can be anywhere in the world, from the moment the patient uses device 33, the data will arrive on the screen of the doctor from the hospital that made the assignment.
The rule is that the device must always be provisioned by the healthcare provider as part of a remote monitoring program. The sim card is a Vodafone IoT global roaming card powered by Medisanté. We order devices from manufacturers in Taiwan, China and Germany. We put our SIM cards inside.
What will your partnership with Beurer change?
Gilles Lunzenfichter: Our expertise is the cloud. But the day a hospital asks us to deliver 12,000 devices to 14 locations in France within 72 hours, we won’t be able to do it. With Beurer, this will be possible because they make 400 million euros in annual turnover sending devices from China to Germany and anywhere else in the world. Their ability to finance stock, stock devices at the scale required and distribute anywhere in Europe within 48 hours, these were abilities we would never have alone.
Up until now, we had been buying devices on demand from mainly Taiwanese and Chinese manufacturers, but this required a large financing effort, especially since these manufacturers always have a minimum order quantity. Beurer will help us scale up in terms of logistics and device financing, while allowing us to focus on our core business.
What is driving these changes?
Gilles Lunzenfichter: In the next few years, there will be reimbursement codes in Germany, France and Holland for remote medical monitoring. This means doctors will be paid to remotely monitor patients 24/7.
In Germany, they announced a code for heart failure patients in 2022. In France, the reimbursement code for the remote monitoring of chronically ill patients will be introduced in 2023, and Holland will follow. This type of remote monitoring is proven to save money.
In the United States, they’ve been doing this since 2019. They understood that for this to work, you have to rely on devices that bring cellular connectivity to the patient’s home without making assumptions about how they are equipped (smartphone or not, internet or not, etc.) or what they know how to do or not. Because the more assumptions you make, the less it works.
In the United States, the physician is allowed to bill for the telemonitoring service if he or she collects at least 16 measurements per month from the patient. The patient takes the measurements, the data arrives directly on the doctor’s screen and if this is done 16 times a month, then he or she can bill the insurance. It’s $1,300 a year per patient for this insurance, which is advantageous. As a result, in 5 years, 50% of American doctors have done this.
Was it Covid that changed the game?
Gilles Lunzenfichter: Of course. Doctors believed that they were the only profession in the world that didn’t need to go virtual. They were convinced, but the day Covid arrived and they saw their waiting rooms empty for several months, they realized that teleconsultation was becoming mandatory.
But teleconsultation doesn’t use devices and is limited. The next step is really to include devices. In the wake of the pandemic, it has become obvious that telemedicine is here to stay after teleconsultations went through the roof.
The next wave is expected to be remote patient monitoring (RPM) and decentralized clinical trials (DCT), with personal health devices acting as the new data collection motor for healthcare teams’ IT systems. But concerns about security, privacy and inclusion need to be addressed. It is very easy to become extremely vulnerable when connecting patient data.
So how do you ensure maximum security?
Gilles Lunzenfichter: The IoT connectivity modules that we put in our devices with our SIM card are manufactured by Thales and Thales, which is the top security company in the world for connected devices. This is a safety guarantee. A home bluetooth connection is very easily hackable.
In your opinion, does the growing market of objects connected to smartphones and bluetooth have huge potential for security flaws?
Gilles Lunzenfichter: Yes, these objects present huge breaches, that’s why no hospital is going to collect data with a device if it’s not sure of the endpoint. In the future, there will be increasingly strong security requirements from hospital IT teams. Hacking and ransomware risks have become too dangerous.
With our gateway, we can still include bluetooth devices, but with security settings. For example, we don’t let any measurements through if they are from a device we haven’t registered beforehand. In our cloud platform, we know exactly which devices the hospitals we collaborate with have distributed. So if there’s a measurement from a device we do not know, we do not let it pass through. That’s why it has to be the physicians who provide the patients with devices. This allows us to control everything that enters the hospital’s clinical system.

The cybersecurity risk surrounding connected objects in hospitals is already huge. There can be a financial risk, the hospital can find itself completely stuck, etc. And in our industry, that is, devices for remote patient monitoring and connection in the home, the risk is even greater. It’s exponential!
So the only way to reduce the risk of breaches is to do it on a private cellular network, and the only way to have a private cellular network is to do what we do with our security settings. The whole transmission chain must be completely reliable.
What about respect for the patient’s privacy?
Gilles Lunzenfichter: Once Mr. Martin is given device 33, he does not need to enter any information about himself, he simply measures his blood pressure with device 33. Then, the information is sent and immediately our cloud knows that device 33 has been given to him by the Timone hospital in Marseille and the data must be sent to that hospital. And in Marseille, they know that device 33 belongs to Mr. Martin.
So when the blood pressure data from device 33 enters the Timone hospital in Marseille, it is automatically assigned to Mr. Martin’s patient file. Patient privacy is fully respected as no patient identity or information that would make a patient identifiable is shared with any device manufacturer or with us. This is also our strength.
We have already been integrated with 50 remote monitoring systems in Europe. We exceeded one million in turnover last year and today we have about 10,000 connected devices.
Our goal is to reach 100,000 connected devices in the next two years and the partnership Beurer will help us scale up in terms of logistics and device financing. This will also be made possible by the remote monitoring reimbursement policies that are emerging throughout Europe following the Covid-19 pandemic. Because Covid-19 made it clear that remote monitoring is the future of medicine for chronic and elderly patients.