A 16-year-old cancer patient has been given a state-of-the-art, fully customized scapula implant in a pioneering collaboration between digital technology and healthcare experts.
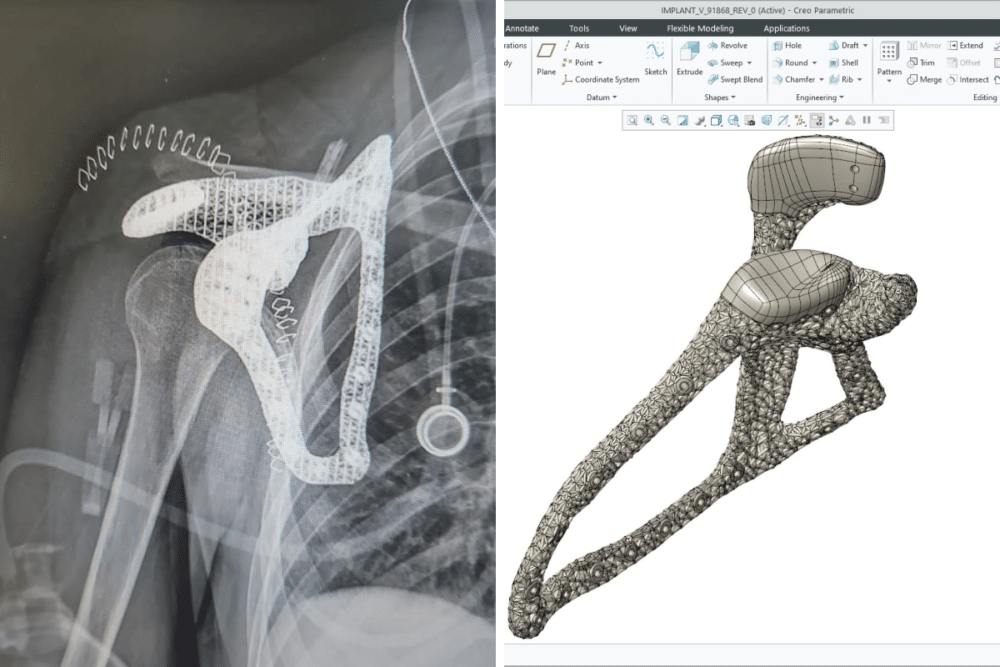
The girl was being treated for a high-grade, malignant tumor. She received a 3D-printed, bioactive, titanium implant after her own shoulder blade was removed.
The collaborative project saw engineering technology come together with personalized healthcare to design and create the scapula to fit seamlessly into her body and permit function and mobility.
The team included experts from the Levin Center for 3D Printing and Surgical Innovation at Tel Aviv Sourasky Medical Center, global software company PTC and simulation software designers Hexagon.
Dr. Solomon Dadia, Orthopedic Oncology Surgeon and Head of the Surgical Innovation and 3D Printing Unit, Tel Aviv Sourasky Medical Center, said:
“You will not see this kind of collaboration in any other hospital. An operation like this, with this depth of understanding of biomechanics and effort into restoring function, has never been done before.”
Dr. Ronen Ben Horin, VP Technology at PTC, added:
“We not only worked with the medical team to find a solution but we provided them with the most cutting-edge technology that humankind has to offer.”
Taking Technology into Theater
The development of complex, implantable, printed materials, together with powerful additive manufacturing and simulation software, has enabled surgeons to employ smart implants, explained Dr. Dadia.
“These implants interact with tissues to optimize their survival in the body, ensuring a perfect fit and promoting tissue growth.”
The team conducted a 3D segmentation of the girl’s tumor and surrounding bone to facilitate effective reconstruction.
A digital twin of the anatomical model was created. It was printed at a 1:1 scale to assist in preoperative planning and delineate the resection margins.
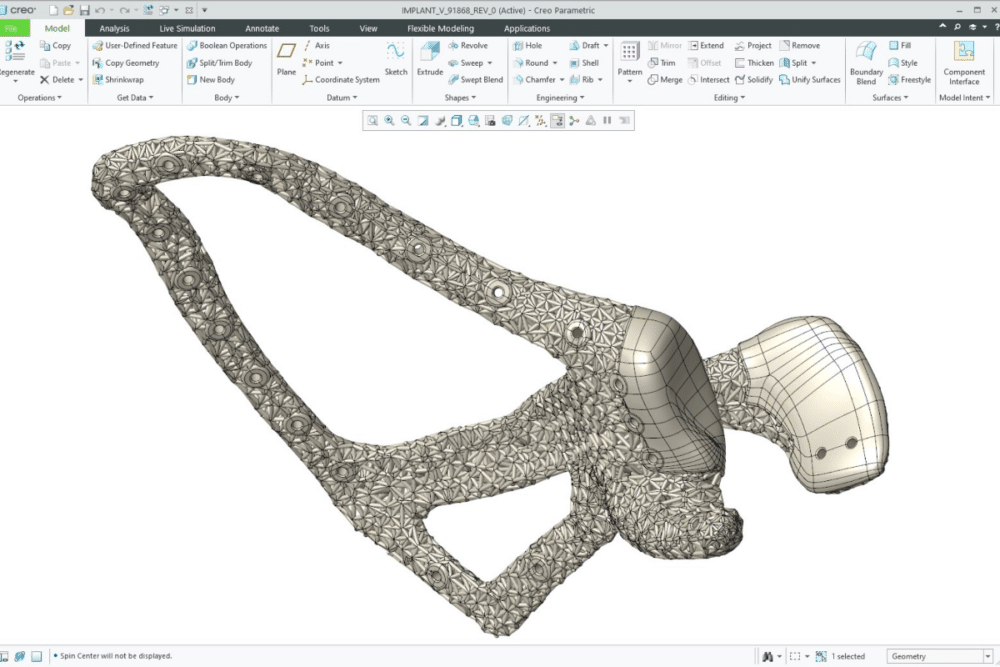
At the same time, the 3D-printed advanced lattice implant was designed (using PTC Creo software) to facilitate the ingrowth of connective tissue and provide anchorage for remaining muscle stumps.
“Eight years ago, when I was working at Imperial College in London I encountered 3D printing and software to segment and reconstruct tissues for the first time. I took it back to my operating theater and started to print models and patient-specific instruments to guide my procedures. From there it evolved to printing metal and polymer implants and now it has got to a point where the Levin Center is a leader in the field. The reason for this is that we take all the technology into a hands-on scenario. Most other European centers stop at the research level and don’t take it further and go into surgery.”
A Strategic Partnership
Dr. Ben Horin explained he and Dr. Dadia teamed up after realizing what they could achieve together.
“At PTC we have great tools for designing sophisticated, latticed parts and using metal materials – all these things are common knowledge in aerospace but not in medical. We wanted to find a way to bring our cutting-edge technology to the medical world. For me, this was very interesting: I am very familiar with how an engineer designs automotives, trains, solar turbines and even spacecraft, but I had never designed an implant. What we have achieved here is to take two different superpowers and make them collaborate in a way that they understand each other.”
A Successful Operation
The 16-year-old patient, who had a sizeable Ewing sarcoma, initially underwent several cycles of chemotherapy in a bid to reduce the tumor, Dr. Dadia explained.
“Unfortunately, however, the tumor was still into all the bone and we decided we had to resect the scapula. The scapula is quite a unique bone – it is a site of insertion for almost 20 muscles that go from the back to the abdomen and shoulder. When you detach all those muscles and do not reconstruct – which is what we normally do and is the standard in all other oncology units around the world – then you lose activity and function in the shoulder site.”
It took just four days from initiating the design of the bioactive, titanium scapula to sending it to the 3D printer.
“If we outsource a custom implant it can take two months, but here we can do it all within one to two weeks. Having the hospital as a manufacturer saves money – it also saves surgical and planning time.”
The operation, which took five hours in total, was a success, Dr. Dadia said:
“It was only three months ago and already we have seen the patient start moving through physiotherapy. She is getting better and better – and we have never seen this before in this kind of huge resection of the scapula bone.”
Dr. Dadia and Dr. Ben Horin now hope more hospitals across the world will move towards increased use of this level of digital technology within their procedures. For Dr. Ben Horin,
“The aim is to make it even cheaper, faster and better, so it can be used by anyone. This is about taking cutting-edge design from industries, such as aerospace, and applying it to a specific person – and it is important to make it common knowledge.”