With brain-machine interface technology now developing rapidly, neuroprosthetics—implants containing multi-contact electrodes that can replace certain nerve functionalities—have the potential to work miracles. They may be able to restore amputees’ sense of touch, help the paralyzed walk again by stimulating spinal cords and silence the neural activity of people suffering from chronic pain.
For decades, researchers have eyed neuroprosthetics as a way of circumventing neural deficits caused by disorders, disease or injury. Today, several different types of surgical brain implants are being tested for their ability to restore some level of function in patients with severe sensory or motor disabilities. Will McGuire, President and CEO of Los Angeles-based neuroprosthetic company Second Sight said:
“This is an exciting time in neuroprosthetics, with advances in technology driving growing adoption. We are seeing devices applied to disorders ranging from pain and restricted movement right through to sleep apnea and vision.”
Visionary Technology
Of the five human senses, sight and hearing are often considered the most important. They allow us to interact with each other and our environment, and the loss of either can be hugely detrimental to quality of life. Building on research into how images and sounds are transmitted and represented in the brain, scientists are now developing neuroprosthetic technologies that can at least partially restore these senses.
Second Sight has developed a series of increasingly advanced implants capable of improving the vision of sight-impaired individuals. The company’s first device, Argus II, is a retinal implant providing vision to individuals with retinitis pigmentosa (a genetic disorder of the eye).
>>>> Read more about Argus II here.
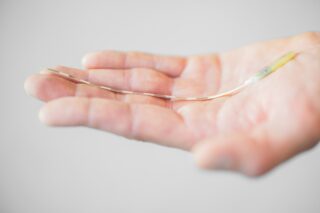
Second Sight’s latest, more powerful product is the Orion Visual Cortical Prosthesis System (Orion). Designed to provide useful artificial vision to individuals blinded by everything from glaucoma and diabetic retinopathy to optic nerve disease and eye injury, it converts images captured by a miniature video camera mounted on a pair of glasses into a series of small electrical pulses.

“Bypassing diseased or injured eye anatomy, the device wirelessly transmits these electrical pulses to an array of 60 electrodes implanted on the surface of the brain’s visual cortex,” explained Will McGuire. “This can provide perception of patterns of light.” Currently undergoing a feasibility study, Orion is now in the FDA pipeline for commercialization. McGuire added:
“Future development may see the number of electrodes increased, the addition of a second camera to aid with distance perception and thermal imaging as well as integrated object and facial recognition capabilities.”
Challenges and Opportunities
As brain-machine interfacing is a hugely complex proposition, developers of neuroprosthetic devices still face multiple challenges. Dr. Robert Flint, a neurology professor at Northwestern University in the United States, explained:
“It is very difficult to interpret brain activity recorded outside the skull with any great detail. Recording brain signals from inside the skull is, in many ways, more desirable. But to acquire signals in this way it is obviously necessary to penetrate the skull. This is really the primary obstacle standing in the way of progress.”

Improving brain-machine interfacing is now the goal of multiple neurotech startups such as Paradromics, Neuralink and Kernel. Despite the challenges, neuroprosthetics have huge clinical potential, with the market expected to display a year-on-year growth of 14% until 2026. Going forward, devices will become smaller and smaller, with more sophisticated arrays, longer battery life and greater use of wirelessly transmitted data and power.
Long-term datasets, recorded over a period of years with the participation of individuals who have implanted approved medical devices like deep brain stimulators, will also become available. This will help the machine learning side of the field with the development and refinement of new control algorithms.