Tech entrepreneur Ayush Jain, CEO of Mindbowser Inc., discusses the next era of digital healthcare with AI diagnostics and connected healthcare.
Clinical care is gradually expanding beyond the hospital walls. According to hospital technology implementation data from Definitive Healthcare, as of February 2024, 78.6 percent of hospitals in the United States had installed a telemedicine solution. This widespread implementation is indicative of a structural change in the way healthcare is delivered, where digital technologies like IoT-enabled gadgets and AI-powered diagnostics are no longer optional extras but are instead becoming essential to patient care.
The variety of digital health devices that are currently being used in clinical settings is evidence of how quickly healthcare is advancing. Cases of technology that are no longer regarded as experimental include wearable biosensors that provide real-time drug monitoring, AI-enabled stethoscopes that can detect heart problems in a matter of seconds and RNA-based home diagnostics for early cancer detection. These technologies are already being introduced into clinics, hospitals, and in some cases, even homes.
Enhancing Diagnostics Using Artificial Intelligence
In the field of diagnostics, artificial intelligence is progressing expeditiously by integrating decision support into instruments that physicians already use. Researchers at Imperial College London have developed an AI-enabled stethoscope that can detect atrial fibrillation and heart failure at an early stage. Instead of being a brand-new gadget, this is an improvement on a conventional tool that allows faster decision-making without altering current clinical procedures.
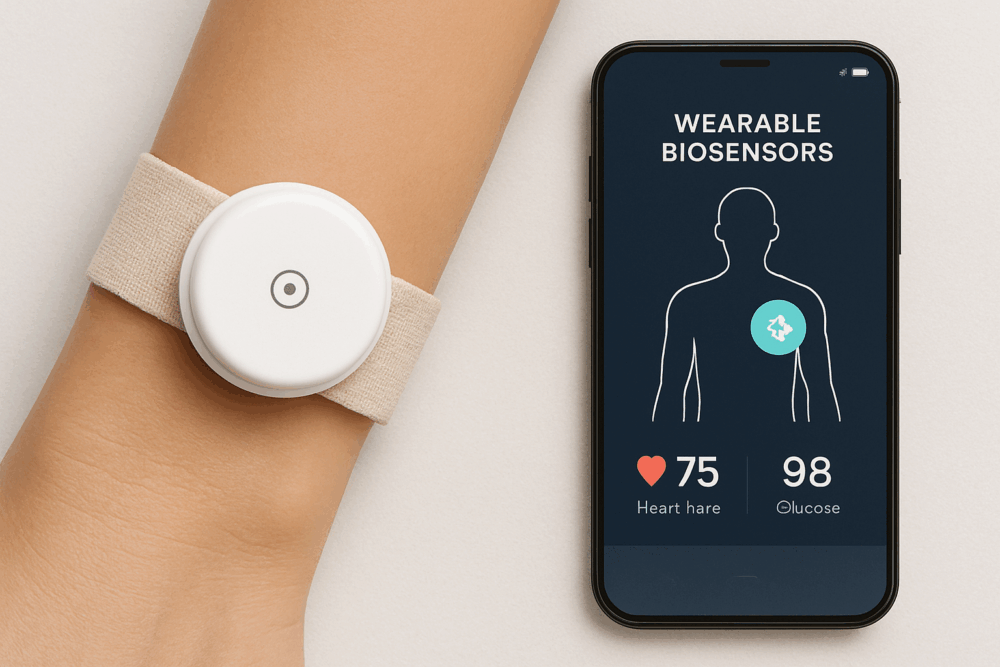
Other applications include ongoing patient monitoring along with point-of-care detection. By tracking biomarkers in real time, wearable biosensors are being developed to give doctors a more comprehensive picture of a patient’s state in between visits. Early trials have shown that these devices can help guide medication dosing more accurately and reduce reliance on repeated blood draws. Instead of being an experimental option, these technologies are increasingly positioned to become a standard component of patient management as regulatory channels develop.

Remote Patient Monitoring Extending Care Beyond Hospitals
One of the most important aspects of chronic care management is remote patient monitoring (RPM). Healthcare professionals can observe patients outside of traditional clinical settings using devices that measure blood pressure, heart rate, or glucose levels. Compared to normal care, patients who use connected monitoring systems have better control over their chronic diseases, according to studies published in npj Digital Medicine. RPM can help healthcare systems cut down on preventable readmissions while giving patients continuity and comfort.
Large-scale initiatives already demonstrate the promise. One of the biggest RPM networks, operated by the U.S. Department of Veterans Affairs, allows individuals to contribute daily health data from the comfort of their own homes. Participants report greater satisfaction and fewer hospitalisations, according to VA News. Compared to intermittent testing, continuous glucose monitors connected to smartphone apps enable patients and doctors to make prompt modifications, which frequently results in better glycemic control. These cases highlight how RPM provides specialised care in remote or underserved locations without necessitating regular in-person visits.
Managing the constant flow of data and ensuring uninterrupted clinical workflows are the two key challenges to address in case of increased usage. Transforming raw data into usable insights requires interoperable health records and analytics advancements. When incorporated into medical procedures and backed by funding models, RPM can transform from a useful supplement to a vital component of managing chronic illnesses.
IoT-Enabled Medical Devices Supporting Connected Care
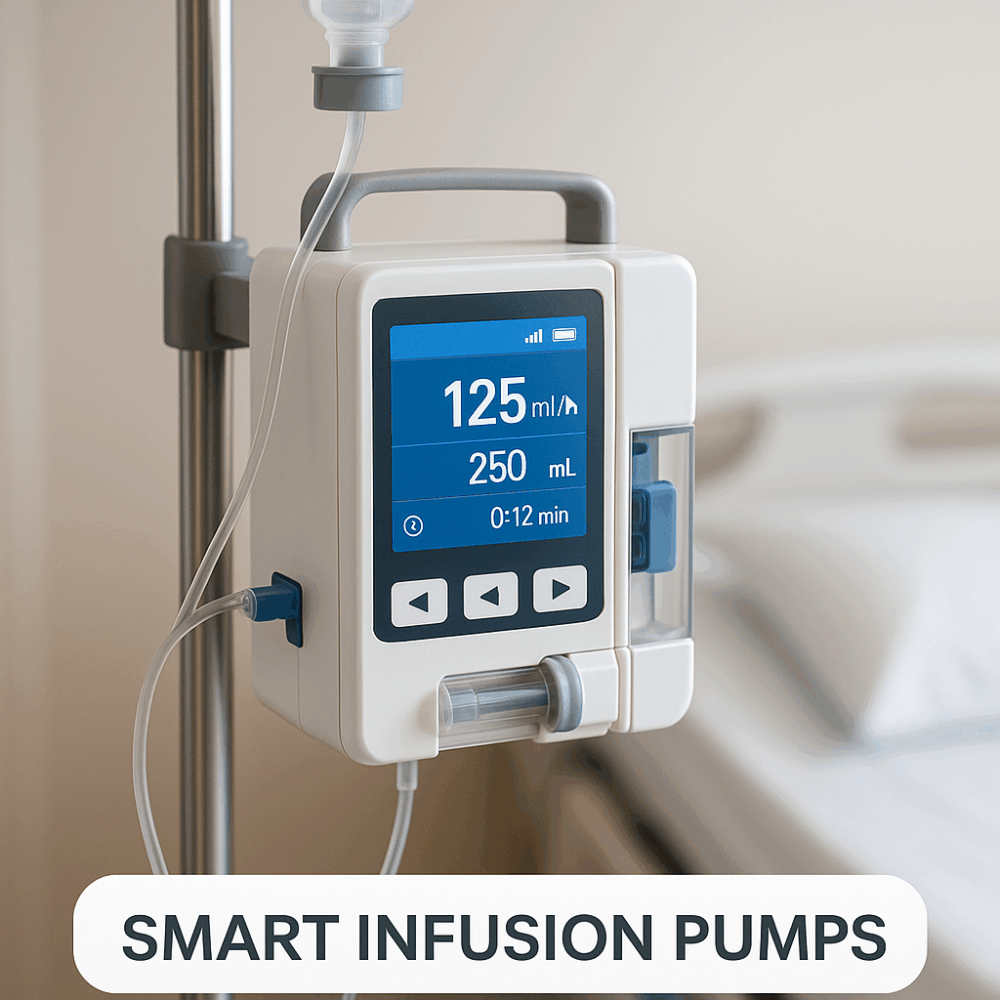
The incorporation of IoT devices into clinical workflows is creating more connected care ecosystems. Healthcare professionals now receive real-time data from connected inhalers, wearable heart monitors and smart infusion pumps. The constant flow of information makes it possible to take prompt action before the complications arise. This information flow lowers the need for frequent hospital visits and aids in the early identification of issues. Medical professionals may make more accurate and well-informed judgments while preserving patient safety and supervision when they combine continuous data with platform interoperability.
This increasing dependence on connected technologies is seen in the market outlook. According to MarketsandMarkets, the global medical device reprocessing market is expected to increase from USD 2.0 billion in 2022 to USD 3.9 billion by 2027, at a compound annual growth rate of 13.7 percent. Hospitals and clinics are searching for sustainable and affordable solutions while regulatory support helps propel adoption. With connected devices becoming a standard part of clinical practice, the potential risk of infection underscores the need for rigorous quality standards to ensure both safety and efficiency.
Integrating Innovation with Equity
The developments impacting digital healthcare today indicate that infrastructure and geography will no longer be barriers to medicine in the future. The potential of AI-powered diagnostics, RPM and IoT-enabled devices to enhance results and decrease needless hospitalisations is already being witnessed. However, overcoming systemic obstacles including clinical training, equitable access and interoperability is important to their overall effectiveness. These technologies may continue to operate as standalone tools rather than as a seamless component of the continuity of care if they are not integrated into electronic health records and reimbursement models.
According to WHO, disparities in internet access and digital literacy continue to be major obstacles, despite the fact that digital health solutions can help close gaps in underdeveloped areas. In the United States, telemedicine has expanded quickly in metropolitan hospitals, but adoption is sometimes constrained in rural areas by network problems. To ensure that linked health solutions serve all populations, not just those with access to digital technology, policymakers and healthcare professionals must find a balance between innovation and inclusion.
Shaping the Next Phase of Care
Digital health technologies are no longer considered to be confined to healthcare. AI-powered diagnostics, remote monitoring systems, and IoT-enabled devices are a few such tools that have already proven improvements in patient care and clinical accuracy. Their expanding use is indicative of a consistent change in care concepts away from intervention-only approaches and toward ones that prioritise continuity and prevention. The current challenge is integrating these tools into routine healthcare systems in a way that is sustainable for providers and useful for clinicians.
Further, this progress needs to be inclusive in order to be meaningful. The extent to which these developments are used will depend on the availability of dependable internet, reasonably priced devices, and patient-professional training. Although technology is heading in an appropriate direction, its effects will be determined by how well healthcare systems are able to spread their advantages outside of urban areas to the areas that most need them.