Medha Nicky Rishi, Founder and CEO of MissPoppins, a parenting and health tech platform, provides insights into telehealth for clinic, post-surgery, and general health consumer support.
Telehealth has radically transformed the way families and patients receive care. Findings show that the percentage of physicians using telemedicine increased from 43% before the COVID-19 pandemic to 88% after it (CDC, 2024). This rapid rise in adoption is not just a trend, it’s becoming a necessity, especially for parents navigating the early stages of family life or patients recovering from surgery.
The Lack of Post-Surgery/Health Support at Home
In the post-surgical landscape, families are often discharged from hospitals with pamphlets but no people. Guidance on wound care, mental health support, live consultations for urgent questions, and reminders for follow-up are critical and telehealth meets those needs with unprecedented immediacy.
The most overlooked demographic in this revolution is new parents and families. Parents Magazine recently reported that rural mothers are giving up breastfeeding earlier and not due to lack of will, but lack of support. In some communities, hospitals discharge mothers without even explaining how to monitor a baby’s hydration through diaper counts, as pediatrician and lactation consultant Dr. Lisa Hammer pointed out. These are not small misses, they are massive failures of education and access (Parents, 2025).
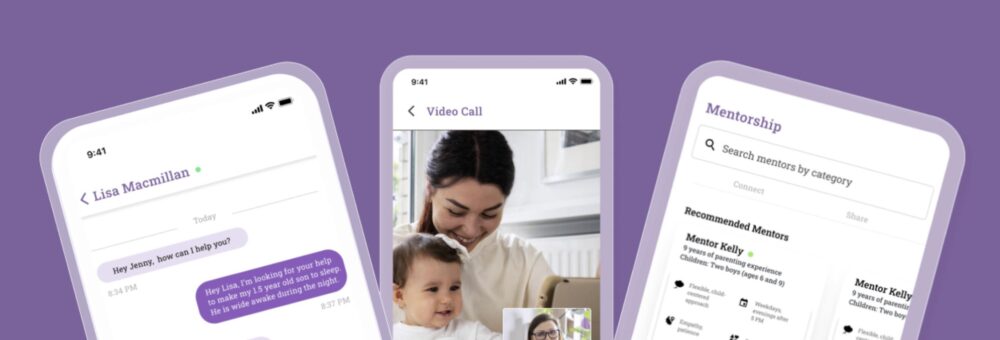
Telehealth apps like MissPoppins can address accessibility issues by offering on-demand access to lactation consultants, grief counselors, sleep coaches, pediatric nutritionists, and doulas, all available through a single, user-friendly platform. Our coaches are culturally aligned and trauma-informed. Across the board, tele-interventions have increased parental engagement and emotional connection, especially in the first year of life.
Dr. Sarah Jane Schwarzenberg, a pediatrician at the University of Minnesota Masonic Children’s Hospital, emphasized the importance of discharge education, particularly post birthing, stating, “We need to make sure that rural mothers are equipped with breastfeeding information and resources before being discharged from the hospital” (Parents, 2025).
I noted in the Parents article that telehealth is expanding rapidly, offering parents flexible, on-demand support from prenatal through toddler stages. Virtual care goes beyond just being an educational handbook; users can get guidance on wound care, live video consultations for urgent questions, recovery checklists, calendar reminders for follow-ups, mental health support, and reduced transportation costs and/or time of work. These tools not only simplify recovery but also ensure families aren’t navigating complex health situations alone.
Current Barriers to Access for Healthcare
As someone who spent over a decade leading global HR, including as Head of HR at Square, I know that employees aren’t just seeking benefits, they’re seeking flexibility, relevance, and dignity. When I became a mom to twin boys, I found myself breastfeeding at 3 a.m. while also preparing to lead executive meetings at 9. That’s when I realized something profound: the systems meant to support us weren’t built for the realities of modern caregivers. So I founded MissPoppins, a digital village powered by AI and expert human guidance to ensure parents no longer have to navigate those moments alone.
Many support categories, such as speech therapy, are also in high demand with long waitlists. In the U.S. alone, over 73% of speech therapy professionals report having a waitlist, according to a ScienceDirect study (ScienceDirect, 2024). For rural and underserved families, these wait
times can mean months without needed care. Telehealth platforms can reduce waitlist times, offering on-demand support with an interactive marketplace for providers.
Changes in Employee Benefit Health Incentives
The recently passed “One Big Beautiful Bill” further enables this evolution. Starting in 2025, employers can offer first-dollar coverage of telehealth services under high-deductible health plans (HDHPs) without impacting HSA eligibility. This legislative shift reinstates a pandemic-era “safe harbor” and opens the door for telemedicine to be treated as primary care, not a backup plan.
Telehealth, or telemedicine has experienced rapid evolution as workplaces seek to maintain employee retention and boost wellness outcomes. According to the 2022 KFF Employer Health Benefits Survey, 95% of firms with 50 or more employees offering health benefits now include telemedicine which is up from 85% the previous year and 67% three years prior.
Yet, utilization rates remain low when benefits are generic. As I shared recently with Canadian HR Reporter, the shift we need is toward hyper-personalized benefits: Instead of taking contributions out of your paycheck toward benefits that aren’t applicable to you, let employees choose. That boosts morale, utilization, and retention. The article also highlighted the growing trend in adaptable health benefits. Organizations are realizing that benefits must evolve beyond one-size-fits-all perks to deeper, targeted support systems. Other top global HR executives by profession weighed in on the issue.

Modern Healthcare is Accessible for All
Telehealth isn’t just about convenience. We’ve seen the dark side of telehealth’s commodification. Platforms that promise speed but under-deliver on care quality are burning out clinicians and eroding trust. The recent U.S. Senate investigation into pharmaceutical companies’ use of telehealth for mass prescriptions is a warning sign. We must resist the temptation to scale without a soul. That’s why at MissPoppins, we enforce clinical guardrails, uphold therapist safety, and focus on long-term impact over short-term metrics.
We must resist the temptation to scale without a soul.
I often return to the Japanese concept of ikigai, the convergence of what we love, what we’re good at, what the world needs, and what we can be paid for. MissPoppins lives at that intersection. We are not just scaling tech; we are scaling empathy. Whether you’re recovering from surgery or welcoming a newborn, virtual care ensures that no one goes through it alone.
The future of healthcare is not just digital, it’s deeply personal. And if we do this right, we won’t just treat patients. We’ll support people. At every stage, in every household, for every family.
All of this begs a larger question: what should modern care look like? I believe the answer is deeply human. It looks like a new mom texting a lactation consultant without having to leave her couch. It looks like a dad joining a grief circle from his garage during a lunch break. It looks like employers embedding family-first support into their wellness budgets not as perks, but as infrastructure.
Nicky Rishi is the founder and CEO of MissPoppins, a parenting and health tech platform supporting families through AI-powered, expert-led care. She previously led global HR and Benefits for Square and serves as a thought leader on employee wellness, parenting innovation, and inclusive workplace design. Her work is recognized through her active roles for multinational advisory boards. Nicky continues to shape her pursuit of philanthropy, business, social good, and innovation through tech. Follow her @askmisspoppins.