Advanced imaging techniques, particularly CT, are essential for improving the precision and success of heart procedures like TAVR, mitral valve repair, and LAA closure.
In recent years, the role of advanced imaging techniques in heart procedures has grown exponentially. Radiologists are now at the forefront of intricate cardiovascular interventions, offering precise, real-time guidance in complex cases such as Transcatheter Aortic Valve Replacement (TAVR), mitral valve repair, and Left Atrial Appendage (LAA) closure. These procedures, once unimaginable without open-heart surgery, are increasingly being performed through minimally invasive approaches thanks to the integration of cutting-edge imaging technologies.
During a panel discussion at the European Congress of Radiology (ECR), three expert radiologists highlighted the importance of imaging in cardiac interventions, focusing on its indispensable role in preoperative planning, procedural navigation, and postoperative monitoring. Through their insights, the discussion laid bare the value of high-resolution CT scans, multi-planar reconstructions, and software-based simulations in ensuring the success of life-saving cardiac treatments.
Precision Imaging in TAVR Procedures
Dr. Ricardo P. J. Budde from Rotterdam, Netherlands, opened the discussion with an in-depth analysis of imaging requirements for Transcatheter Aortic Valve Replacement (TAVR), an intervention for treating aortic stenosis in patients who are not candidates for open-heart surgery. The focus of his talk revolved around the critical measurements radiologists must make when assessing a patient’s suitability for TAVR, a process that heavily relies on detailed imaging of the aortic root and annulus.
“The aortic annulus is not a perfect circle; it is an ellipsoid structure that requires careful multi-planar reconstruction to ensure accurate measurement,” Budde explained. “Incorrect sizing of the valve can lead to catastrophic complications like valve dislodgment or annular rupture during the procedure.”
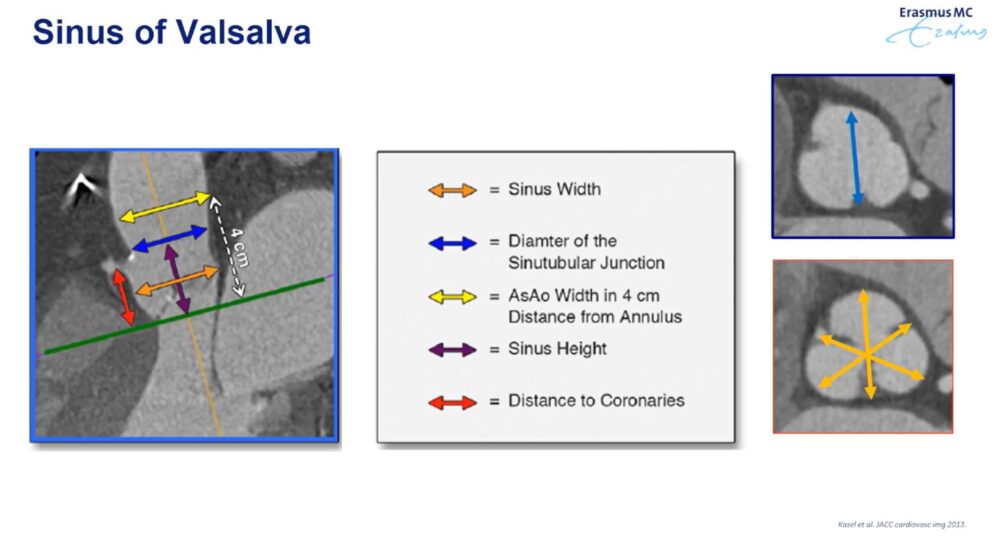
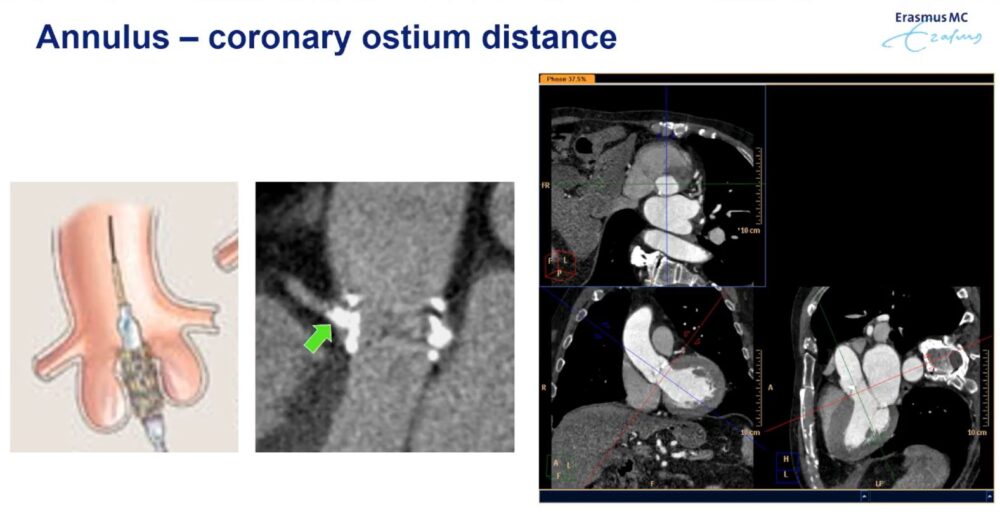
CT imaging plays a pivotal role in determining key parameters such as annulus diameter, the distance between the aortic annulus and the coronary ostium, and the extent of calcification on the native valve leaflets. This precise anatomical information guides the surgeon in selecting the appropriate valve size and determining the safest access route—whether transfemoral, transapical, or direct aortic.
Budde also highlighted the development of new technologies, such as photon-counting CT, which improves the ability to assess coronary arteries in heavily calcified patients. This advance holds the potential to reduce the need for invasive coronary angiography, particularly in elderly patients undergoing TAVR.
Mitral Valve Repair: Complex Anatomy Meets Imaging
Dr. Muhammad Taha Hagar from Freiburg Im Breisgau, Germany, provided a deep dive into the imaging intricacies involved in mitral valve repair, focusing on the complex three-dimensional structure of the mitral annulus and its role in valve function. He explained how CT imaging helps overcome the challenges posed by this complex anatomy, offering surgeons a detailed map of the mitral valve for transcatheter procedures.
“The mitral valve forms a three-dimensional, saddle-shaped structure. To simplify our measurements, we use the D-shaped annulus model, which helps us obtain trigon-to-trigon and septal-to-lateral distances more easily,” Hagar said. “Calcification, while problematic in some cases, can also serve as a stabilizing anchor for the valve.”
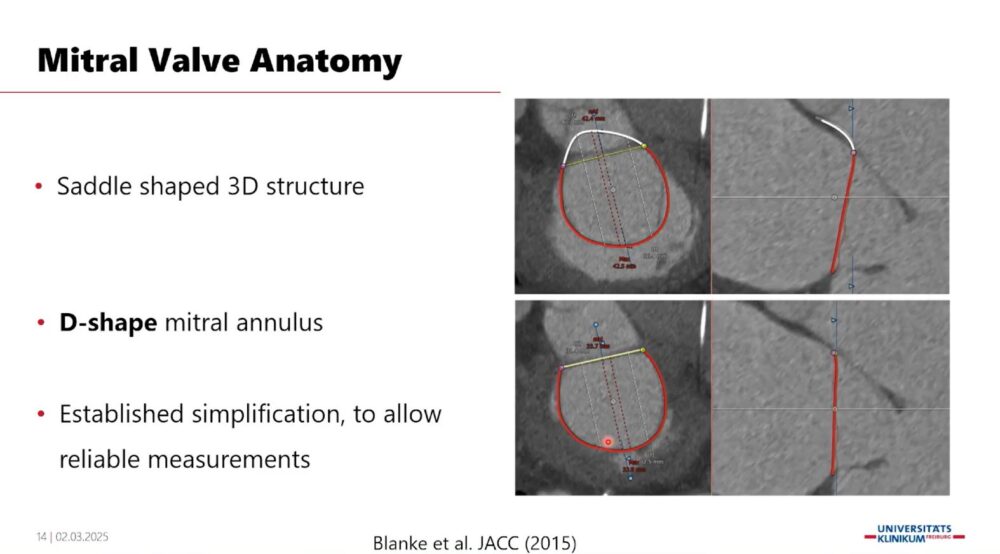
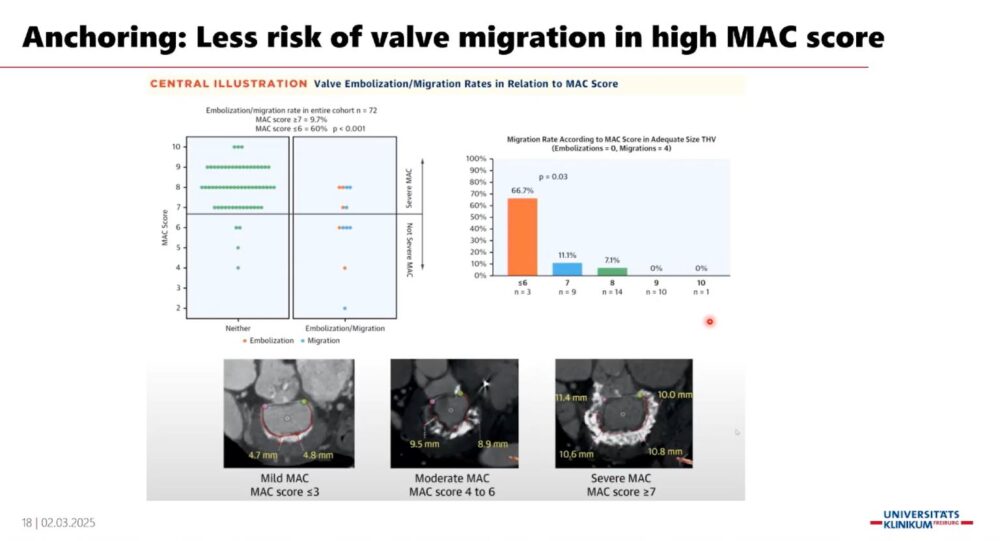
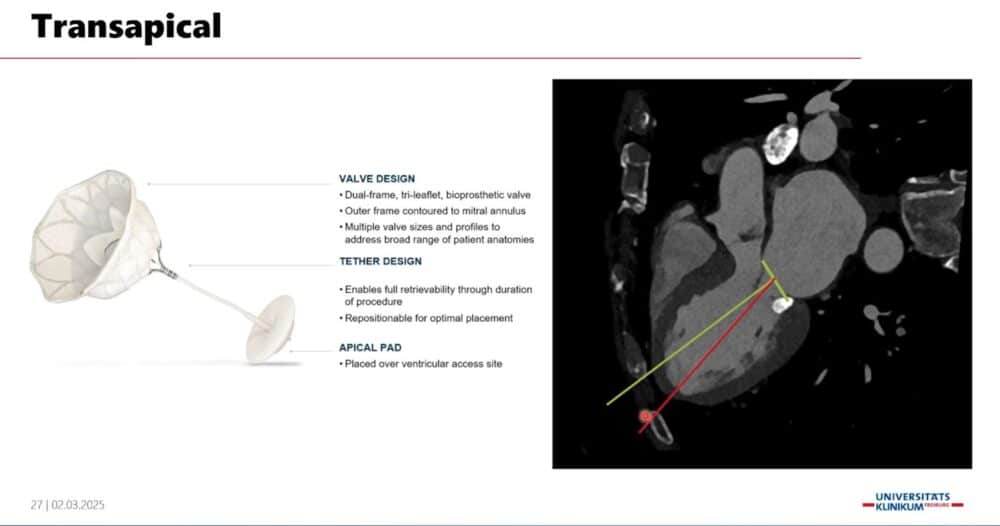
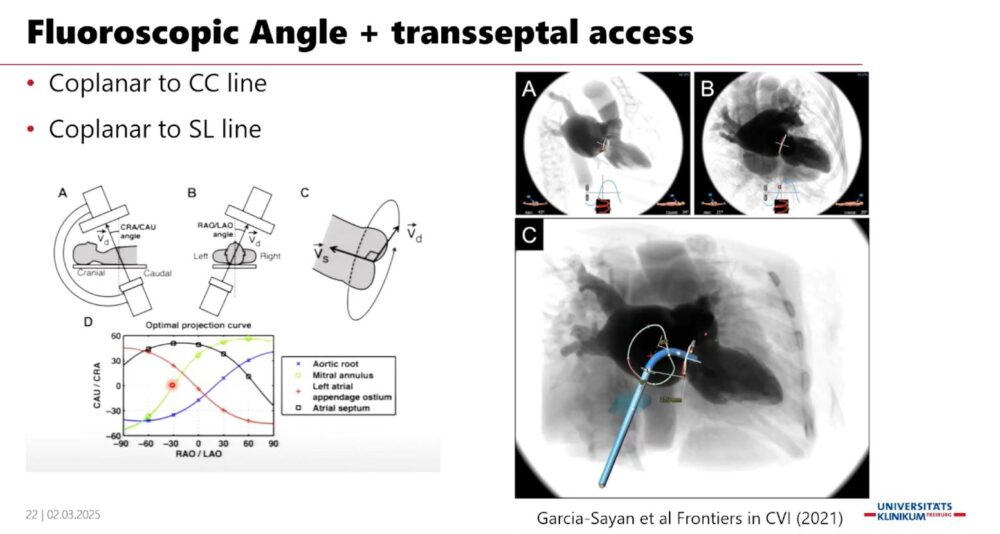
CT-based imaging protocols help identify calcifications and other anatomical features that must be considered when planning the placement of a new valve. Importantly, these images also help predict complications such as left ventricular outflow tract (LVOT) obstruction, which can occur due to the close proximity of the mitral valve to the LVOT. Hagar emphasized that full cardiac cycle acquisition during CT scans is crucial for assessing LVOT dynamics and ensuring safe valve deployment.
“These CT images allow us to simulate the placement of a new valve and evaluate its potential impact on the LVOT before surgery, which reduces the risk of complications,” Hagar noted.
Software-based solutions are increasingly used to assess potential anatomical challenges, providing surgical teams with a comprehensive picture for decision-making.
LAA Closure and AFib: Imaging at the Core of Success
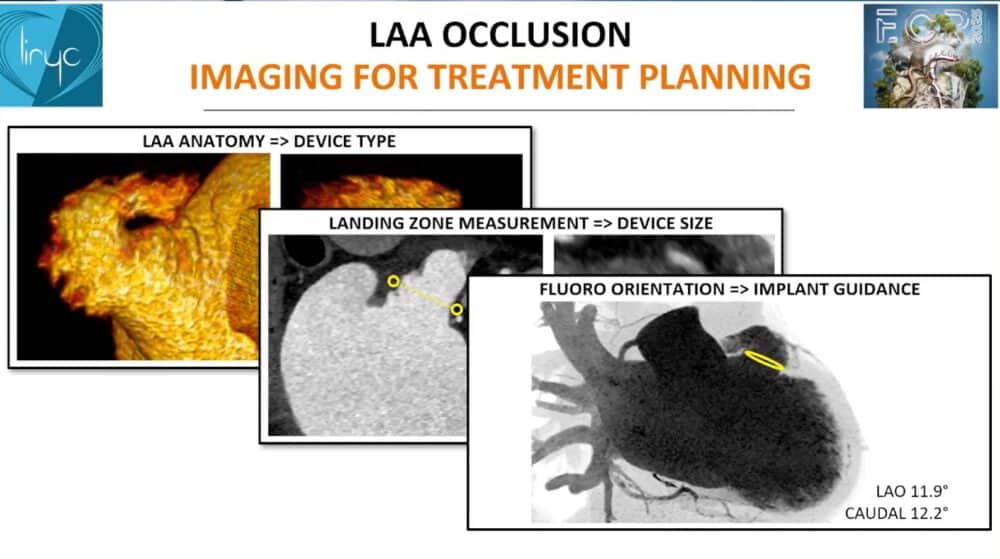
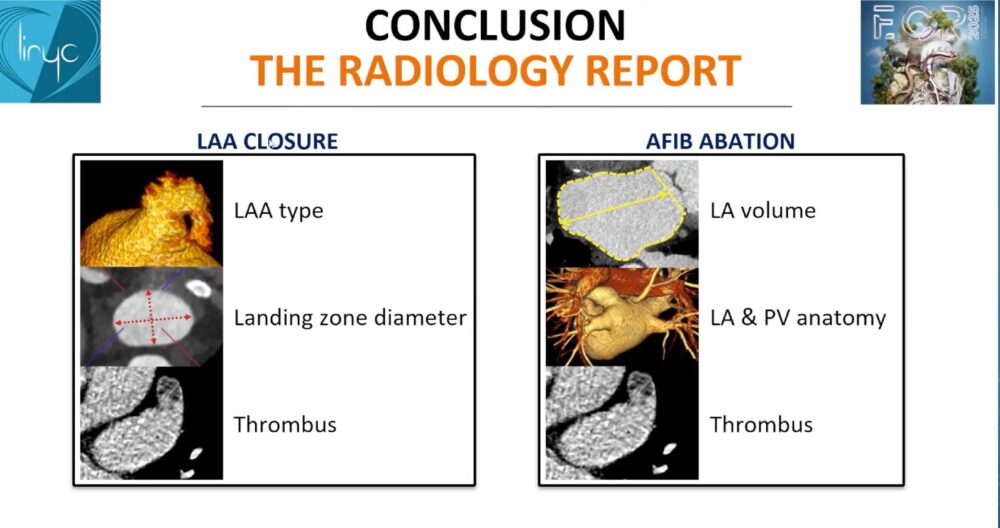
Dr. Hubert Cochet from Pessac, France, shifted the focus to interventions for Left Atrial Appendage (LAA) closure and Pulmonary Vein Isolation (PVI) for atrial fibrillation (AFib). As these procedures target patients with an elevated risk of stroke who cannot tolerate long-term anticoagulation, the success of such interventions is highly dependent on accurate pre-procedural imaging.
“Catheter ablation for atrial fibrillation has emerged as a crucial strategy, with CT imaging guiding both patient selection and the procedure itself,” Cochet said. “In planning for LAA closure, it’s critical to assess the anatomy of the left atrial appendage, determine the landing zone for the device, and rule out thrombus to minimize the risk of embolism.”
Cochet emphasized the role of CT in identifying various LAA shapes, such as the high-risk “chicken wing” LAA morphology, which may influence the choice of closure device. Furthermore, post-procedure imaging is equally important, particularly in detecting residual LAA patency or device-related thrombus formation, which may pose a stroke risk.
“In our series, 5% of patients showed high-grade hypoattenuation related to thrombus formation on post-implant CTs, which is not negligible,” Cochet remarked.
This underlines the essential role of imaging not just for procedural success but for long-term patient monitoring and risk reduction.
Images: Screenshot of the presentation. Courtesy of the speaker and ECR.
As cardiac interventions become increasingly complex, imaging continues to be the linchpin of success. Radiologists, equipped with advanced CT technologies and software solutions, are playing a critical role in guiding cardiologists and surgeons through the delicate anatomy of the heart. From ensuring accurate valve sizing in TAVR to preventing LVOT obstruction in mitral valve repair and minimizing stroke risk in LAA closure, imaging provides a detailed roadmap for precision treatment.
The insights shared at the ECR panel underscore the importance of collaboration between radiologists and cardiac teams, ensuring that patients receive the best possible care with the least invasive interventions.











