Medical professionals discuss how advanced imaging technologies play a significant role in oncology diagnostics during ECR.
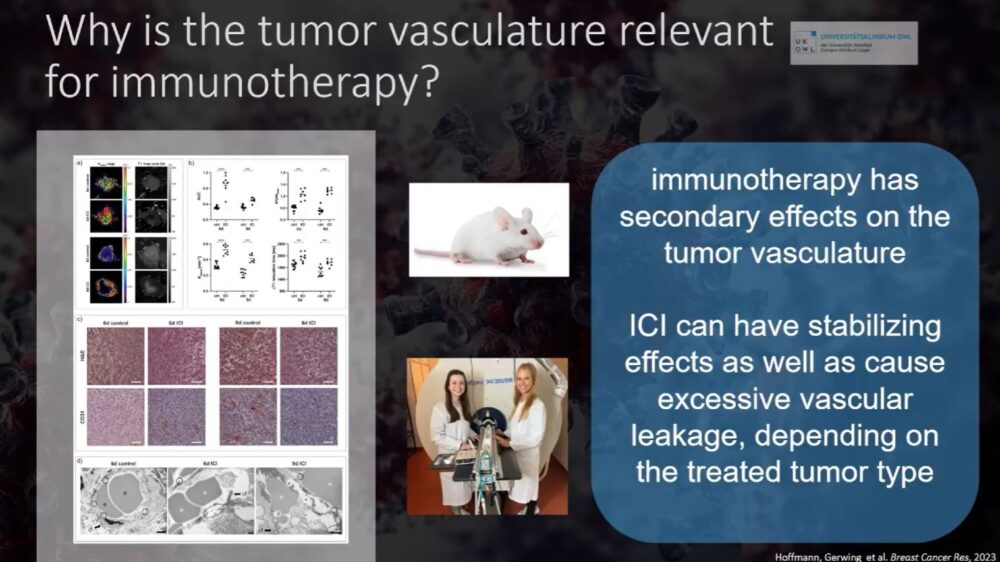
The landscape of oncology has shifted dramatically in recent years, moving beyond conventional chemotherapy toward immunotherapy—a field that harnesses the body’s immune system to target and destroy cancer cells. However, the success of immunotherapy depends heavily on precise patient selection, monitoring, and response assessment. Advanced imaging techniques have emerged as indispensable tools in this evolving paradigm, yet their full potential remains underutilized in clinical practice.
At the recent ECR panel discussion, Imaging Answers to Immunotherapy Demands, experts addressed the critical role of imaging in optimizing immunotherapy outcomes. Here, we focus on the points mentioned by Ass. Prof. Dr. Med. Mirjam Gerwing, MBA, EDiR (University Medical Center OWL, Klinikum Lippe) and Dr. Caroline Lips (Senior Physician, Medical Oncology, Cantonal Hospital St. Gallen). They provided an in-depth look at the state of oncologic imaging today, its limitations, and its promising future.
Current Standard of Imaging in Immunotherapy
In routine oncologic practice, CT scans remain the backbone of tumor assessment, offering a straightforward approach to tracking tumor size over time. PET-CT scans are used selectively to evaluate metabolic activity, while MRI is occasionally employed for soft tissue contrast enhancement and functional assessments.
However, as Dr. Lips noted, conventional imaging has clear limitations when applied to immunotherapy. Unlike chemotherapy, where tumor shrinkage is often indicative of treatment success, immunotherapy responses are more complex—sometimes characterized by initial tumor enlargement due to immune cell infiltration (pseudoprogression) before eventual regression. Moreover, resistance mechanisms and heterogeneous tumor biology further complicate imaging-based response assessments.
“Who tells us what we’re doing is right? We need to do imaging—CT scans—because this is still, today, the most reliable way to know if we’re treating effectively,” Dr. Lips emphasized.
Yet, she also acknowledged that reliance on conventional imaging alone is insufficient, as tumor size changes often lag behind the underlying biological response to treatment.
Clinical Imaging Challenges and the Need for Advanced Techniques
Dr. Gerwing highlighted an essential gap in current practice: imaging is primarily reactive rather than proactive. Most patients undergo serial CT scans to determine response, yet these scans fail to provide the depth of biological insight necessary to predict which patients will benefit from therapy.
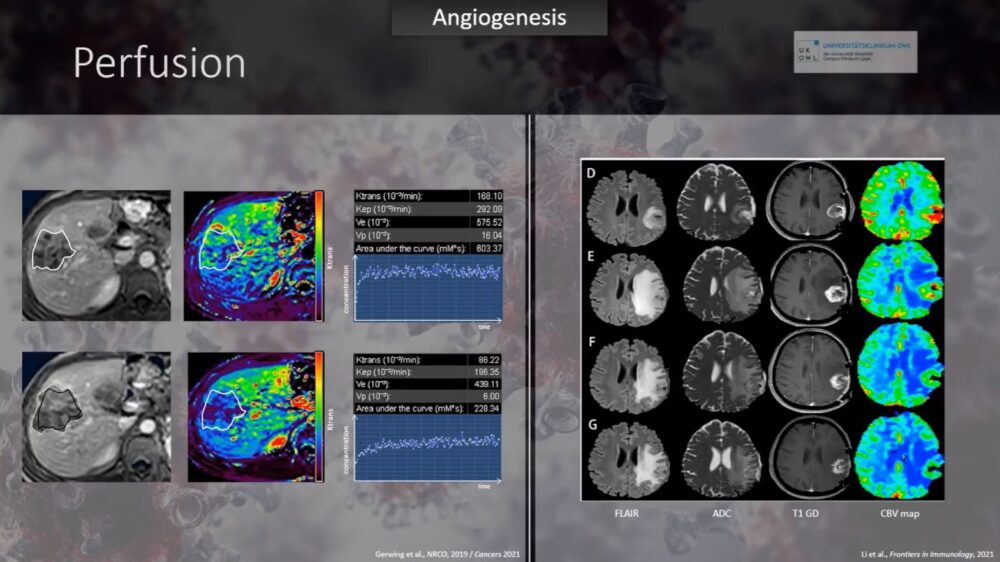
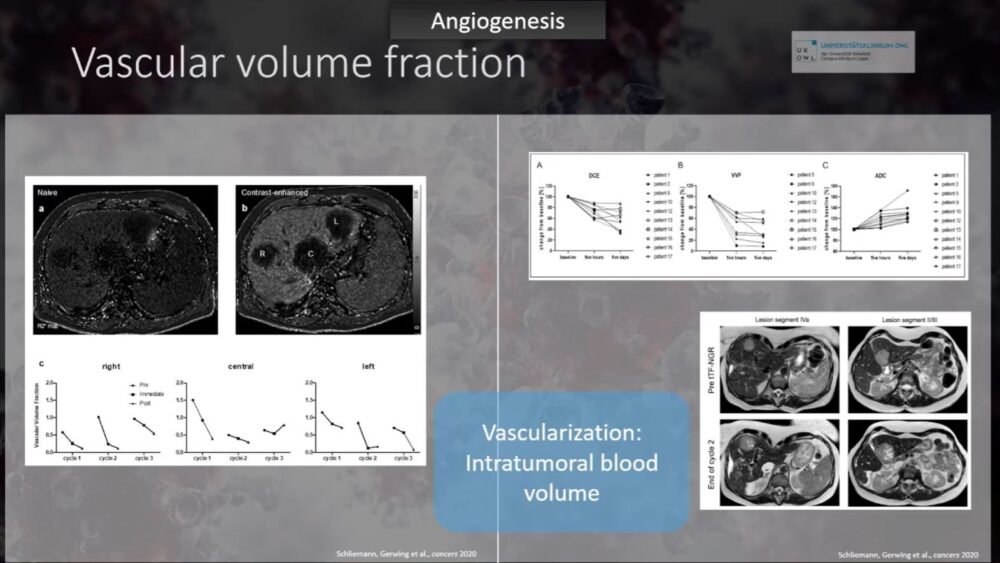
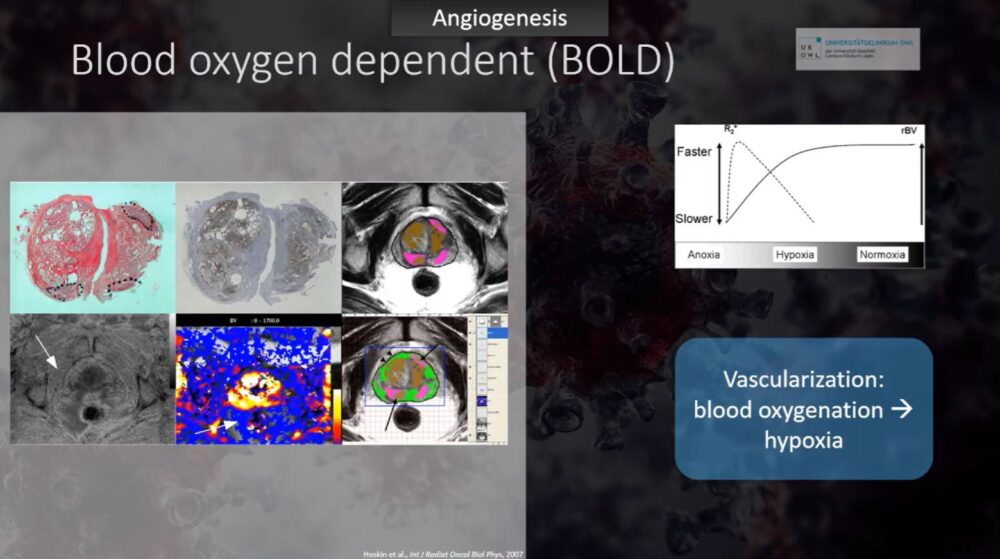
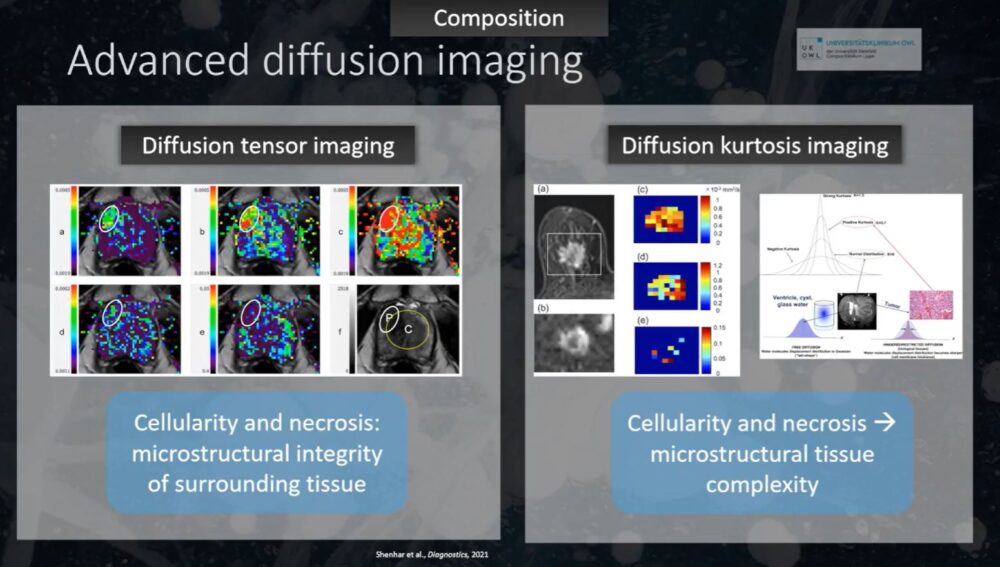
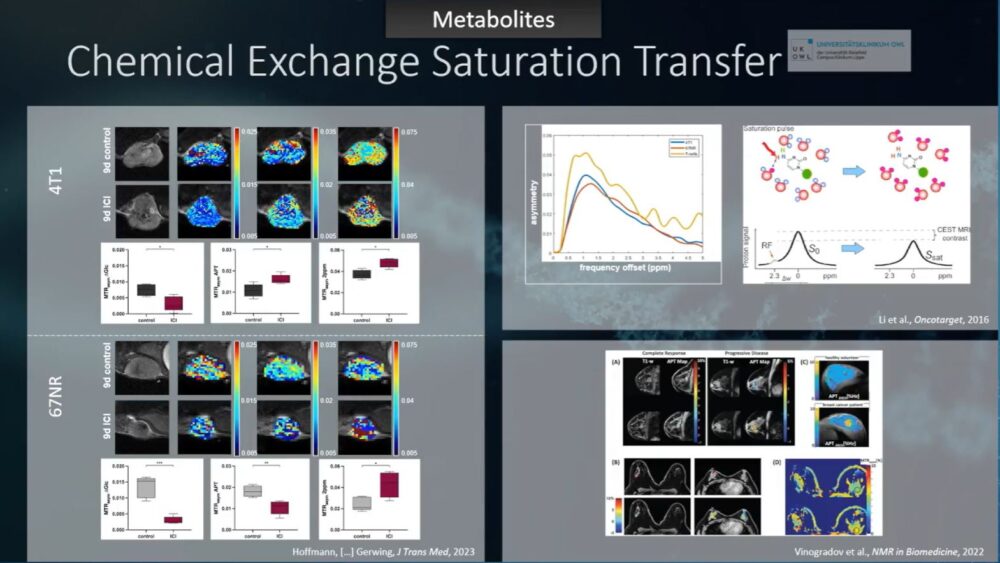
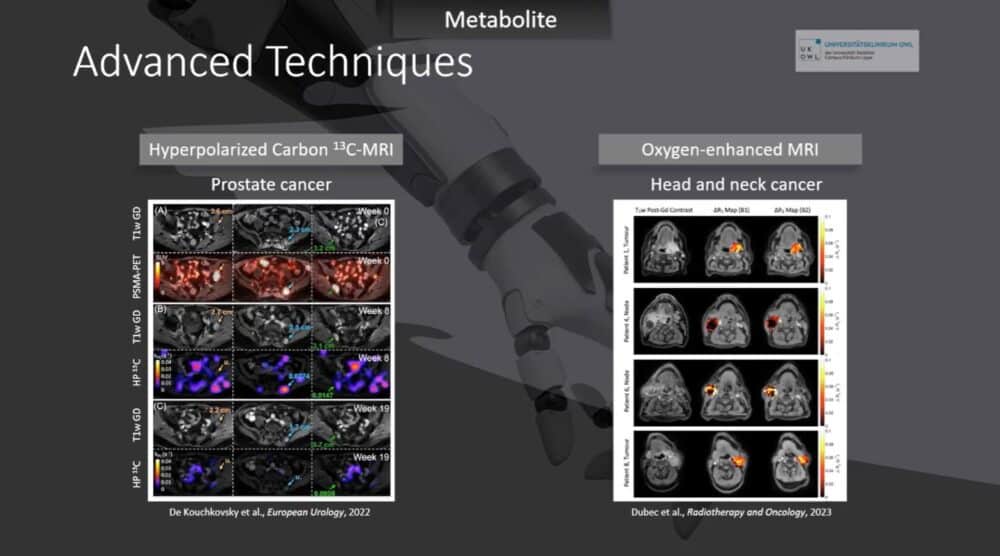
MRI and hybrid imaging techniques offer solutions that could bridge this gap by providing early biological markers of treatment efficacy. Some of the advanced imaging approaches discussed included:
- Dynamic Contrast-Enhanced MRI (DCE-MRI): Allows for real-time assessment of tumor vasculature changes post-treatment, potentially revealing therapeutic efficacy as early as five days after initiation.
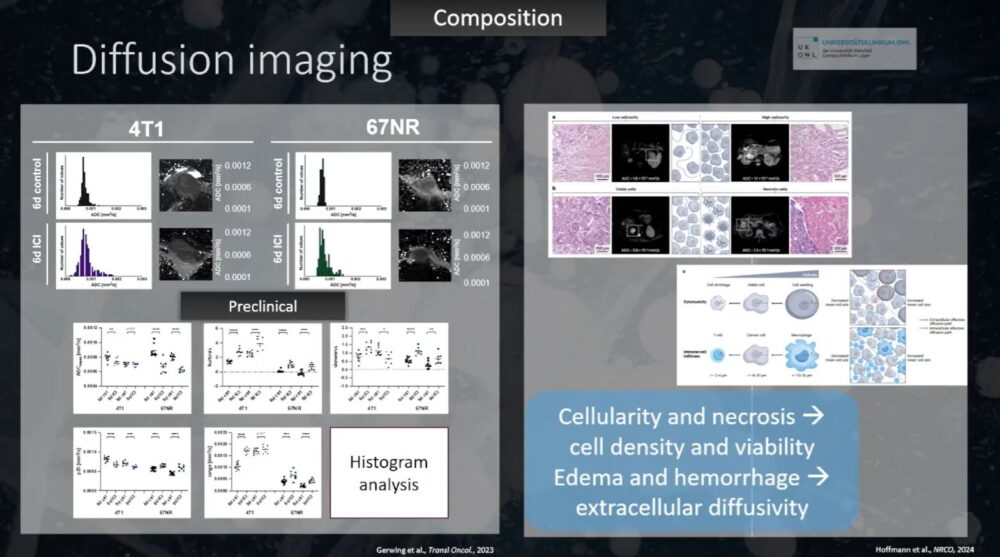
- Diffusion-Weighted Imaging (DWI) & Histogram Analysis: Can detect increased tumor heterogeneity following checkpoint inhibitor therapy, a possible marker of immune activation.
- Arterial Spin Labeling (ASL): A non-contrast MRI technique that can assess tumor perfusion and microvascular invasion, which could guide treatment intensification.
- Blood-Oxygen-Level-Dependent (BOLD) MRI: Detects hypoxia, an essential factor in immunotherapy resistance.
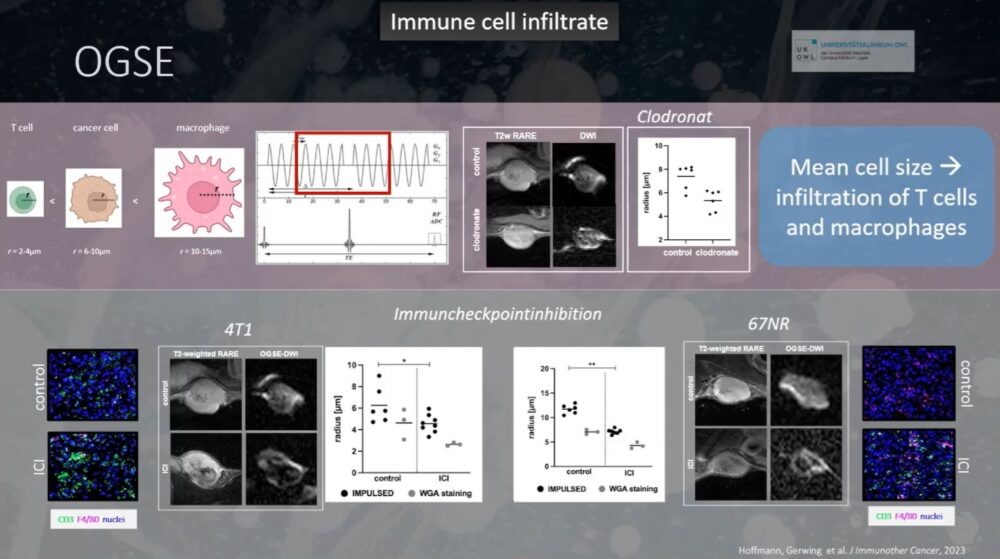
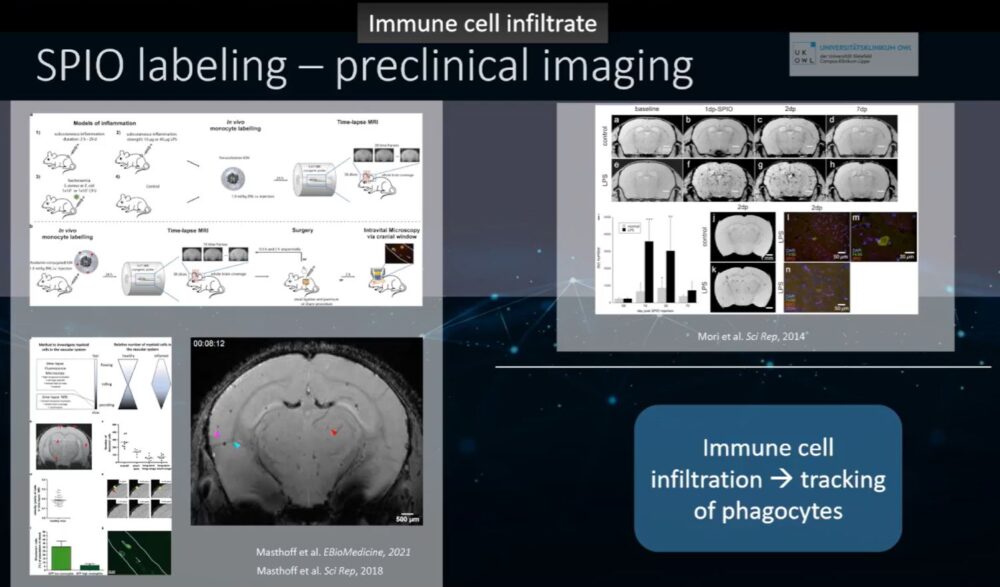
- Pulsed Diffusion MRI with Oscillating Gradients: A cutting-edge, preclinical approach that may help visualize immune cell infiltration at the single-cell level.
“Some of these imaging techniques are readily available, but they are rarely used in clinical routine,” Dr. Gerwing observed. “We have the tools; we just need to integrate them into patient care.”
“We have the tools; we just need to integrate them into patient care.“
The Future: AI, Radiomics, and Precision Imaging
Looking ahead, the next frontier in oncologic imaging will be driven by artificial intelligence (AI) and radiomics. AI-enhanced imaging analysis has the potential to extract vast amounts of quantitative data from standard scans, revealing subtle treatment effects that may not be visible to the human eye.
Dr. Lips pointed to the promise of radiomic biomarkers, which use AI-driven pattern recognition to predict treatment response based on imaging characteristics.
“We do not have reliable biomarkers yet, but radiomics and AI will, I’m sure, revolutionize this in a really important way,” she stated.
Dr. Gerwing further expanded on the vision for the future, suggesting that initial imaging should be far more comprehensive, incorporating multiple MRI sequences to fully characterize a tumor’s biological properties before treatment. Follow-up scans could then be tailored to detect early treatment responses, moving beyond size-based assessments to functional and metabolic imaging.
“My vision is that we have longer MRI protocols at the beginning to understand the tumor, followed by shorter, targeted scans during treatment to assess response,” she explained. “We need to move toward true precision medicine in radiology.”
The Path Forward for Imaging in Immunotherapy
While the tools for advanced imaging exist, widespread adoption into clinical practice remains a challenge. Standardization, accessibility, and reimbursement policies must evolve to accommodate these sophisticated techniques. Multidisciplinary collaboration between radiologists, oncologists, and AI specialists will be essential in translating preclinical imaging innovations into routine patient care.
For now, CT and PET-CT remain the standard, but a future of precision oncologic imaging is within reach. As AI-powered imaging and advanced MRI techniques continue to develop, radiology will play an increasingly central role in tailoring immunotherapy, predicting response, and improving patient outcomes.
“We have to combine AI with imaging to identify the right patients for the right treatment at the right time,” Dr. Gerwing concluded. “That is the future of immunotherapy monitoring.”











