This opinion piece was written by Dr Vikram Ahuja, co-founder and CEO of OsseoLabs.
In recent years, evidence has steadily mounted that the timing of surgery can influence patient outcomes – in ways that may have little to do with the patient or the procedure itself.
A major study published in JAMA Network Open in March 2025 analyzed over 430,000 cases over a span of 13 years. It confirmed something that’s long been suspected in the medical community: patients undergoing surgery on Fridays face a higher risk of adverse outcomes and even death compared to those operated on earlier in the week.
While the increased risk – about 5% – may appear modest, it translates to thousands of preventable adverse events each year when scaled across the millions of surgeries performed globally.
This so-called “weekend effect” has been attributed to multiple systemic factors – among them, for example, the fact that there tend to be less senior clinicians working at the end of the week, as well as less follow-up care over the weekends. And similar disparities show up across other dimensions too – such as geographic location and socioeconomic status.
In 2025, we shouldn’t accept that a patient may suffer poorer surgical outcomes simply based on the day of the week their procedure is performed, or what their postcode is.
But fortunately, change is on the horizon. A new generation of digital tools is helping address these disparities by standardizing a number of factors in surgery that were previously seen as uncontrollable variables.
Reducing The Human Margin of Error
Even the most experienced teams operate within systems that vary widely in their structure and resources. The JAMA study underscores how much a patient’s outcomes can depend on what happens before surgery even begins.
Planning is often the hidden variable. The more optimized this pre-op stage is, the lower the risk once the patient is on the operating table. After all, surgeons often need to make split-second decisions under extreme pressure. However, there are certain things that it traditionally hasn’t been possible to plan ahead of time.

For example, it isn’t uncommon for surgeons to discover the required course of action only after the operation has begun. Think a tumor only found to affect surrounding lymph nodes once the patient is opened up. In cases like this, rapid decision-making in the face of extreme pressure is crucial, and of course, surgeon expertise can make all the difference. But experience shouldn’t be the only thing standing between a good or poor outcome.
Technology can’t completely do away with this variability and its associated risks, but it can help to massively reduce them. For example, AI-enabled surgical planning and computational modeling tools can help teams optimize decisions before a scalpel ever touches skin – enabling teams to map out a precise course of action well in advance.
Leveling the Surgical Playing Field
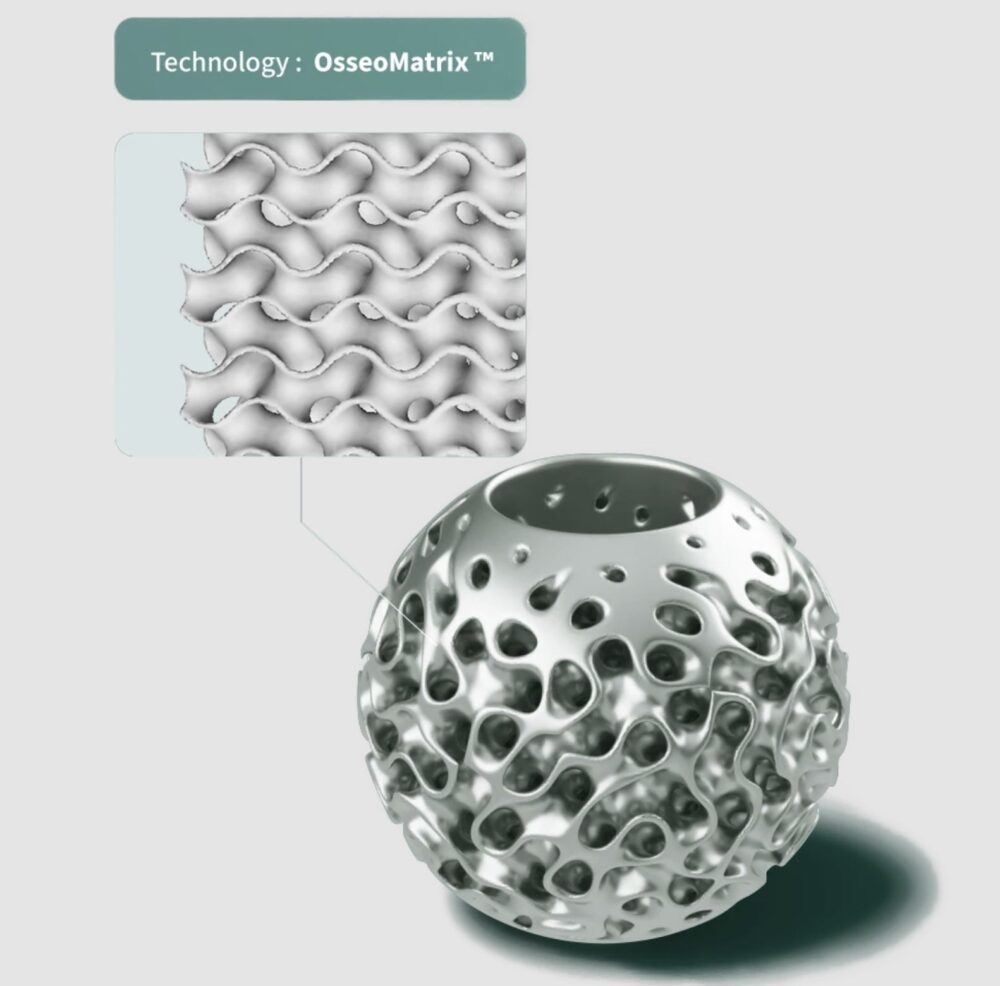
Such technologies reduce the cognitive and procedural burden on surgeons, especially in emergency or low-resource settings. Instead of relying exclusively on institutional memory, surgical teams can make use of data-driven recommendations and custom-printed anatomical models or implants derived from imaging – all of which can be prepared well before surgery begins.
In doing so, AI can help improve and raise the standard of surgical quality across the board, no matter what level of expertise the surgeon has, or what day of the week the surgery is being performed, since far less of the procedure is left to in-the-moment decision-making.
For example, in mandibular reconstructive surgery, it’s not uncommon for a patient to spend hours under anesthesia while a surgeon takes live measurements and fits a custom titanium plate by hand. During this manual process, every minute matters. The longer it takes, the longer the patient is under anesthesia and open on the operating table – meaning greater risk of complications.
But with advanced imaging and AI-based planning, measurements can be taken ahead of time. A patient-specific plate or implant can be 3D-printed to fit precisely – before the patient even enters the OR. Advancement and new applications of AI models in healthcare are significantly shortening the time required to fabricate a patient-specific device. These technologies reduce time under anesthesia, meaning shorter surgeries and hospital stays, fewer complications, and generally more predictable outcomes since less is left to chance.
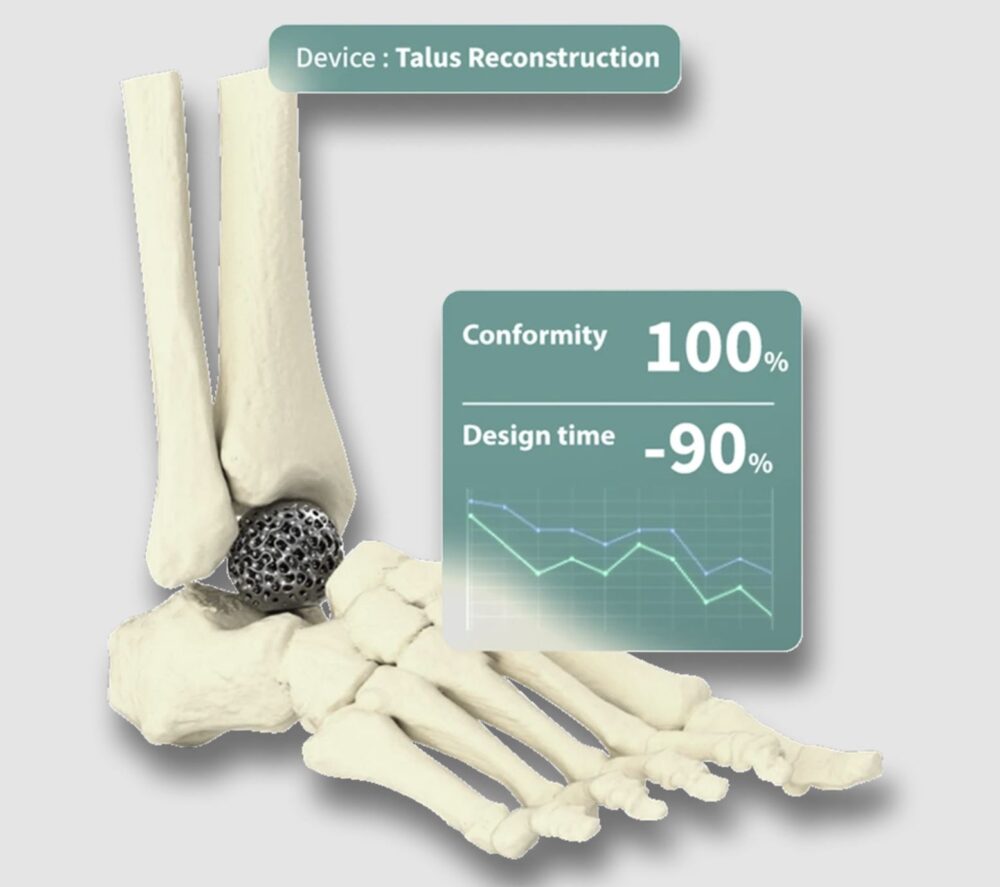
And since procedures become more predictable, this approach supports more efficient resource planning and lower procedural complexity. This means greater access to quality care in underserved regions or institutions where certain surgical capabilities were previously limited.
We recently supported a surgery in a regional Thai hospital where clinicians were performing a complex facial reconstruction – a procedure that would traditionally require significant intra-operative measurement, reshaping, and decision-making under pressure. With our AI-powered workflow, the surgical team received a fully customized implant and surgical plan, based on the patient’s CT scan, before the procedure began.
The result? A 40% reduction in surgical time and a faster, less painful recovery for the patient. In fact, the patient-specific implant meant the patient was able to undergo just one surgical procedure and likely to eliminate any revision surgery for unwanted outcomes.
A New Surgical Standard
While the technology to enable this shift has been available for a few years, the medical industry is slow to utilize and make full use of it. Many hospitals tend to stick with legacy infrastructure and traditional practices since providers are often reluctant to integrate new technologies, despite the clear benefits of AI-enabled workflows.
Furthermore, clinical training programs often lag behind the pace of technological advancement. Regulatory frameworks – especially in the West – are slow to adapt.
Yet, the direction is clear. When surgical planning is enhanced by AI and powered by digital manufacturing, care becomes more consistent and safer. We no longer have to accept that certain patients – whether due to timing, geography, or income – will face worse odds in the operating room.
It’s time to reframe how we think about surgical excellence. The goal shouldn’t be to rely on the best human performance at every moment. It should be to build systems that deliver consistent, data-driven, patient-centered outcomes – regardless of where or when a surgery takes place.
AI will never replace clinical expertise. But it can amplify it and help eliminate the avoidable variability that still increases risk across too many surgical procedures.