Backed by major public investment, Ribeirão Preto’s Nutera Center launches a groundbreaking clinical program poised to cut treatment costs, expand access, and bring cutting-edge cancer care to the country’s public health system
In a hurry? Here are the main takeaways:
- Latin America’s first fully homegrown CAR-T therapy is now being delivered in Ribeirão Preto, Brazil, through the Nutera Center.
- Public investment of over R$ 200 million enabled Nutera to reduce per-patient CAR-T costs to ~R$ 350,000 (US$ 66,000)—far below imported alternatives.
- The Carthedrall Clinical Study (81 patients planned across 5 hospitals) is underway, with Phase 2 authorized in January 2025; early cases show dramatic clinical improvement, though detailed results remain undisclosed.
- Nutera’s CD19-targeted CAR-T protocol uses a 45–60-day vein-to-vein process, followed by inpatient monitoring for inflammatory toxicities.
- International data cited in the article show robust remission rates in refractory B-cell malignancies: 28–68% for lymphomas (2 years) and 62–86% for leukemias (1 year).
- Planned future expansions include trials for autoimmune and neurologic B-cell–mediated diseases, with a lupus study expected to begin in 2026.
For the first time in Latin America, patients suffering from blood cancers are receiving a specific CAR-T cell therapy entirely developed on the continent. This is taking place in Ribeirão Preto, a major city in the Brazilian state of São Paulo, where patients with B-cell acute lymphoblastic leukemia and B-cell non-Hodgkin lymphoma are being treated as part of a scientific study.
The Advanced Therapy Center of Ribeirão Preto (or Nutera-RP, in the Brazilian acronym) was created in 2022. It is the result of a partnership between the Ribeirão Preto Blood Center (chosen by the Brazilian National Health Surveillance Agency, Anvisa, to lead this project for having been, for many years, a reference in cell therapy research in the country), the University of São Paulo (USP), and the Butantan Institute. Both the state government and the federal government invested over R$ 200 million (around US$ 37 million) in Nutera’s infrastructure, supplies, and technical staff.
The investment is considered very strategic for the development and independence of Brazil’s health sector, but reducing the costs involved in this sort of treatment is also crucial. Today, treating a patient with CAR-T therapy can cost up to US$ 500,000, without hospital expenses. As a consequence, the treatment is not yet available in the Brazilian public system, and approximately 120 people only have benefited from this technology in the country since 2019. Meanwhile, over 30,000 patients in the United States and 10,000 in Europe have been treated with CAR-T cells. As the largest and most advanced cancer treatment program in Latin America, Nutera’s mission is to help change that reality. So far, thanks to its efforts, the cost per patient in the ongoing Carthedrall Clinical Study has been R$ 350,000 (or US$ 66,000). Nutera says that the center will soon have the capacity to treat more than 300 patients per year with its new CAR-T technology.


How Nutera’s CAR-T therapy works
The CAR-T cell therapy is based on the use of the patient’s own immune cells to treat blood cancers. The first person to demonstrate its viability was the Israeli immunologist Zelig Eshhar, in 1989. After that, groups in the United States worked on perfecting the manipulation of the cells and the safety of the therapy and began to apply it experimentally to terminally ill cancer patients in the early 2010s. The positive results led the Food and Drug Administration (FDA) to unanimously approve the use of CAR-T therapy to combat cancer in 2017. In the following year, the treatment earned James P. Allison and Tasuku Honjo the Nobel Prize in Medicine.
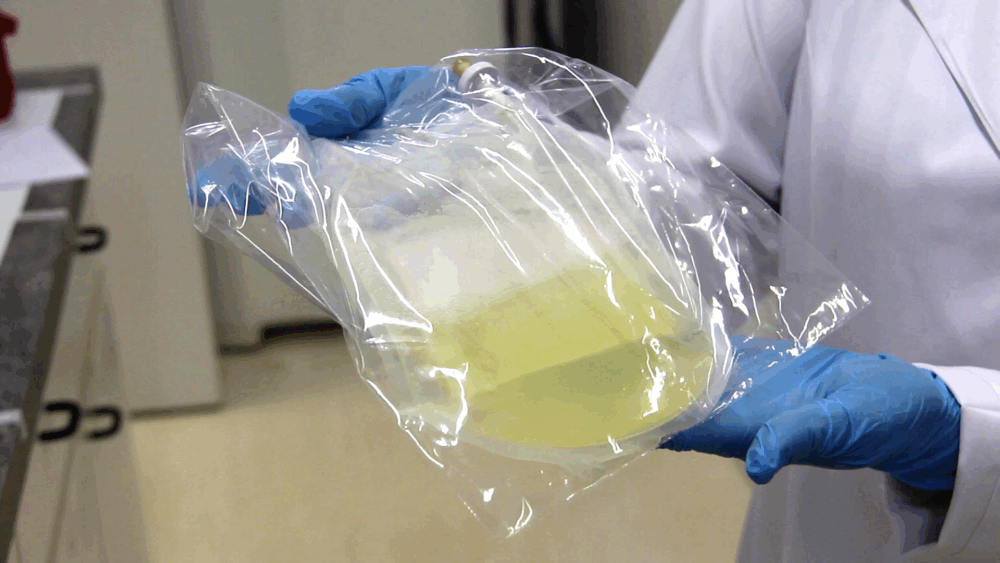
The therapy done in Nutera works in the following way: the patient’s blood is collected and goes through an hours-long process that isolates the T-cells, a type of white blood cell that fights infections in different ways. Then, these T-cells are genetically engineered, with the scientists adding a new gene to them through the use of a modified, deactivated virus. This gene’s function is to create a chimeric antigen receptor (CAR) on the T-cell’s surface, and these CAR proteins are designed to chemically recognize and bind to the CD19, a specific antigen that can be found only on the surface of B-cells (healthy or tumoral). The B-cells are central in this therapy because both B-cell acute lymphoblastic leukemia and B-cell non-Hodgkin lymphoma result from the abnormal proliferation of B-cells. Next, the engineered T-cells are cultivated for at least 10 days in a nutrient-rich liquid until they multiply into tens of millions. After this, the cells are frozen and go through a quality control process that makes sure the cells are not carrying viruses, bacteria, or fungi. Then, the patient needs to be prepared to receive the CAR-T cells through a five-day-long, light type of chemotherapy that eliminates the patient’s existing T-cells. This process—the lymphoid depletion—is a crucial step for the success of CAR-T cell therapy, as it creates an optimal environment by reducing tumor load, removing immunosuppressive cells, and making cytokines (small proteins that act as chemical messengers for our immune system) available for the CAR-T cells to expand and persist. Then, the patients rest for two days before having the CAR-T cells infused into them. Once the CAR-T cells bind to the cancer cells, they trigger the tumorous cells to die.
The whole process—from the collection of the blood to the infusion of the CAR-T cells—lasts between 45 and 60 days. After receiving the CAR-T cells, patients must stay in the hospital for proper monitoring and control of the inflammatory response occurring in their bodies. As these CAR-T cells can remain in the body for a long time, they end up providing a sustained immune response against the cancer, potentially creating long-term remission.
Carthedrall: the ongoing research
Nutera’s Carthedrall Clinical Study has received so far R$ 100 million (around US$ 18 million) in funding from Brazil’s Ministry of Health. Started in 2024, Carthedrall aims to treat 81 people in five reference hospitals. These patients have B-cell acute lymphoblastic leukemia or B-cell non-Hodgkin lymphoma and are either experiencing a return of the disease or did not get better with standard treatments like chemotherapy and bone marrow transplants.
Until Nutera’s Carthedrall Clinical Study, the CAR-T therapy had only been offered in Brazil to 20 individuals on an experimental and small scale, from 2019 onwards. The excellent results were published in 2024 in the magazine Bone Marrow Transplantation and helped support the request for authorization for the Carthedrall trial.
Carthedrall Clinical Study has two phases and was granted authorization to start its second phase in January 2025. This allowed Nutera’s partner hospitals to recruit and treat patients, who will be monitored by the medical team for five years. Dr. Diego Villa Clé, hematologist and coordinator of both Nutera and the Carthedrall Clinical Study, estimates that a fourth of these 81 patients will have been treated by December of this year and that the second phase of the study should end by the second semester of 2026. Due to legal reasons, Nutera cannot yet disclose the results of the ongoing study, but Dr. Villa Clé says that there have been cases of dramatic improvement in the patient’s situation.
“There are many challenges. This technology is so complex that this is the first time the entire process has been done in Brazil. Then, the next big challenge was transitioning from the world of academic research at a university, where those first 20 patients were treated just one at a time, towards a factory structure capable of taking this technology to the public system. We only overcame this challenge thanks to our partnership with Instituto Butantan and the creation of Nutera. And the current challenge is the clinical study itself. These diseases are extremely serious; many patients simply cannot wait those 45 to 60 days and die waiting for the treatment,” Dr. Villa Clé told MedicalExpo e-Magazine.

A Therapy with Superior Results & Nutera’s Aims for the Future
Among the advantages of CAR-T cell therapy are a reduction in chemotherapy sessions and in pain medication and a greater chance of complete or partial remission of the disease. In a review article published in 2023 in the journal Nature Reviews Clinical Oncology, researchers from the American National Cancer Institute (NCI) stated that, in the case of lymphomas, the rate of participants in whom the disease became undetectable two years after CAR-T treatment ranged from 28% to 68%. In leukemia, between 62% and 86% showed no signs of the disease one year after infusion. And it is important to remember that these patients had not responded well to previous treatments and, in most cases, were in a very critical condition.
Although Nutera’s focus now is on blood cancers, the idea is to expand, in the future, the use of the cell therapy to autoimmune diseases that involve malfunctioning B-cells, such as lupus, rheumatoid arthritis, and systemic sclerosis.
“Nutera already has a study targeting lupus, which is waiting for an authorization from both the surveillance agency and the Research Ethics Committee. The resources are already guaranteed, and this study must start in 2026,” says Villa Clé.
Another potential use for Nutera’s CD19-targeting CAR-T cells is in treating neurological diseases that affect B-cells, such as myasthenia gravis and neuromyelitis optica.










