Dr. Douglas Romer provides information on tech-based approaches to hypertension care, referencing NICaS impedance cardiography and MedsEngine for sustained blood pressure control rates.
This article was written by Dr. Douglas Romer
Primary Care Physician | Chief Medical Officer, MedsEngine
Primary care is facing one of its most defining moments. With chronic disease rising, clinician capacity stretched, and health outcomes stagnating, the question isn’t whether we need to do better—it’s how. One of the clearest opportunities for improvement lies in a condition that affects nearly half of U.S. adults: high blood pressure.
Hypertension is the primary contributor to the world’s leading causes of death, heart disease and stroke1. Despite decades of innovation in medication, blood pressure control in the U.S. remains poor. According to CDC data, control rates dropped to 43.7% by 20182, and under newer guidelines using <130/80 mmHg as the target, that rate is closer to 20%. This represents not just a public health concern, but a clinical opportunity.
A Data-Backed Model with Remarkable Results
Two large primary care groups—PriMED Physicians in Dayton, Ohio, and Premier Medical Associates in Pittsburgh, Pennsylvania—have utilized a technology-based approach to hypertension care that dramatically improves control rates. Using NICaS impedance cardiography (Tel Aviv, Israel) and MedsEngine clinical decision support software (Dayton, Ohio), these practices have reported sustained blood pressure control rates as high as 92% for 10 consecutive years3.
The data have been presented at leading international meetings, including the 2023 and 2024 European Society of Cardiology Congresses and the 2025 European Society of Hypertension meeting3,4,5.

29 August – 01 September 2025
Madrid, Spain & Online
What Makes This Approach Different?
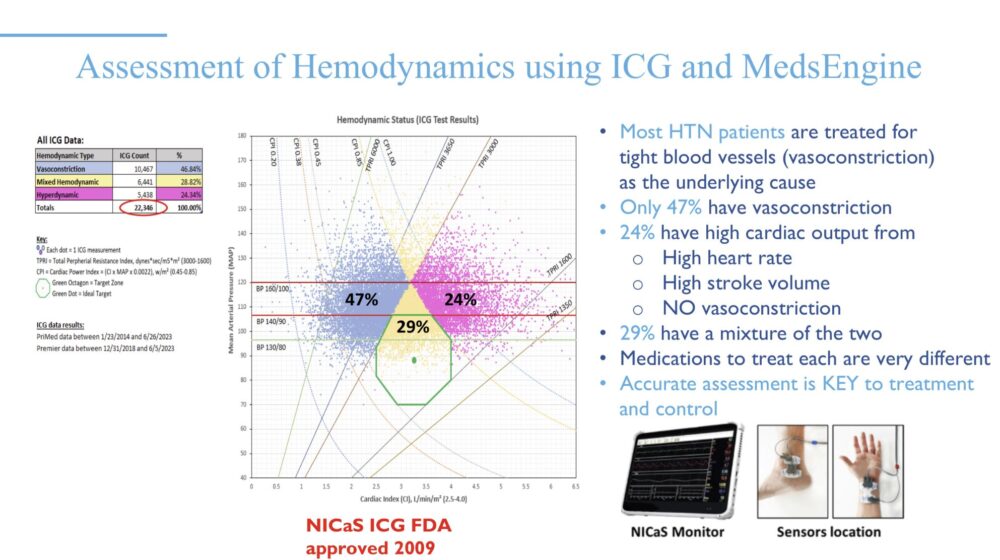
Both practices use noninvasive hemodynamic testing to determine the underlying cause of each patient’s hypertension. NICaS identifies abnormalities across three key physiologic drivers:
- Vasoconstriction (tight blood vessels)
- Elevated cardiac output (from increased heart rate or stroke volume)
- Increased intravascular fluid volume
In a cohort of over 14,000 patients and 22,000+ NICaS tests, results showed:
- 47% of patients had isolated vasoconstriction
- 24% had hyperdynamic circulation
- 29% had a mixed profile3
This data contradicts the widely held assumption that vasoconstriction is the primary cause of elevated blood pressure.
Translating Data Into Actionable Care
Both groups also utilized MedsEngine, a clinical decision support tool that analyzes over 35 patient-specific variables to recommend a personalized antihypertensive medication. The software generates a visual report that displays the source of the patient’s high blood pressure and the rationale behind the treatment plan.
This visual education component has significantly improved patient adherence. When patients can “see” their blood pressure problem and understand the logic behind treatment, engagement rises—resulting in more consistent follow-through and improved outcomes.
These results are real. They’ve led to measurable reductions in heart attacks and strokes within these patient populations. And importantly, this approach is not confined to academic centers. It’s primary care–driven, efficient, and replicable.
With tools like NICaS and MedsEngine, blood pressure can be brought to goal in less than two office visits, on average5. That efficiency matters—not just for physicians, but for patients navigating chronic conditions in fragmented systems.
The Future of Primary Care is Personalized
Themes emerging from recent international conferences are clear: precision, personalization, and better data at the point of care. The answer is not more medications. The answer is using technology, with the medications already available, tailored to the individual.
Hypertension is just one example of what’s possible when primary care steps into the future. The tools are available. The outcomes are documented. What remains is broader adoption.
About the Author
Dr. Douglas Romer is a board-certified primary care physician and the Chief Medical Officer of MedsEngine. His work focuses on precision-driven solutions for chronic disease management. He has presented internationally on data-backed approaches to hypertension care. Learn more at MedsEngine.
Sources
1. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet: Volume 398, Issue 10304, P957-980, September 11, 2021
2. Trends in Blood Pressure Control Among US Adults with Hypertension, 1999-2000 to 2017-2018. JAMA Published online September 9, 2020
Paul Muntner, PhD; Shakia T. Hardy, PhD; Lawrence J. Fine, MD; Byron C. Jaeger, PhD; Gregory Wozniak, PhD; Emily B. Levitan, ScD; Lisandro D. Colantonio, MD, PhD
3. A physiologic, precision-medicine approach to guided pharmacological treatment of hypertension substantially improves blood pressure in a large community-based cohort
European Society of Cardiology Congress 2023, Amsterdam, Netherlands. August 25-28
Romer, Vered, Cleland, Froehlich, Perez, Colangelo, Crossey, Bottorff, Matthews, Hardtke, Kaiser, Granov, Sobotka
4. Pharmacologic treatment of hypertension guided by non-invasive haemodynamics in primary care improves blood pressure control. European Society of Cardiology Congress 2024, London, England, August 29–September 1, 2024. Romer, Cleland, Sobotka, Matthews, Kaiser, Granov, Froehlich, Perez, Colangelo, Crossey, Bottorff, Hardtke, Vered
5. Haemodynamically-guided selection of therapy improves blood pressure control efficiently in primary care. European Society of Hypertension 2025, Milan, Italy May 23–26, 2025. Romer, Cleland, Vered, Sobotka, Granov, Kaiser, Froehlich, Perez, Colangelo, Crossey, Gearhardt, Bottorff, Viera