Researchers at the University College of London developed a diagnostic algorithm for the treatment of drug-resistant epilepsy.
Around 50 million people worldwide suffer from epilepsy, a brain condition that causes recurrent seizures of various types. While anti-seizure medication is available and effective for most people with this disorder, between 20% and 30% of patients don’t respond.
Although there is still a lot of ongoing research on the disorder, an abnormality of the brain called focal cortical dysplasia (FCD)—identifiable by MRI scans—is considered to be one of the leading causes of drug-resistant epilepsy. Recent studies have shown that of all patients suffering from FCD, only 20% respond to anti-epilepsy medication; whereas for all the total cases of epilepsy, this number is around 70%.
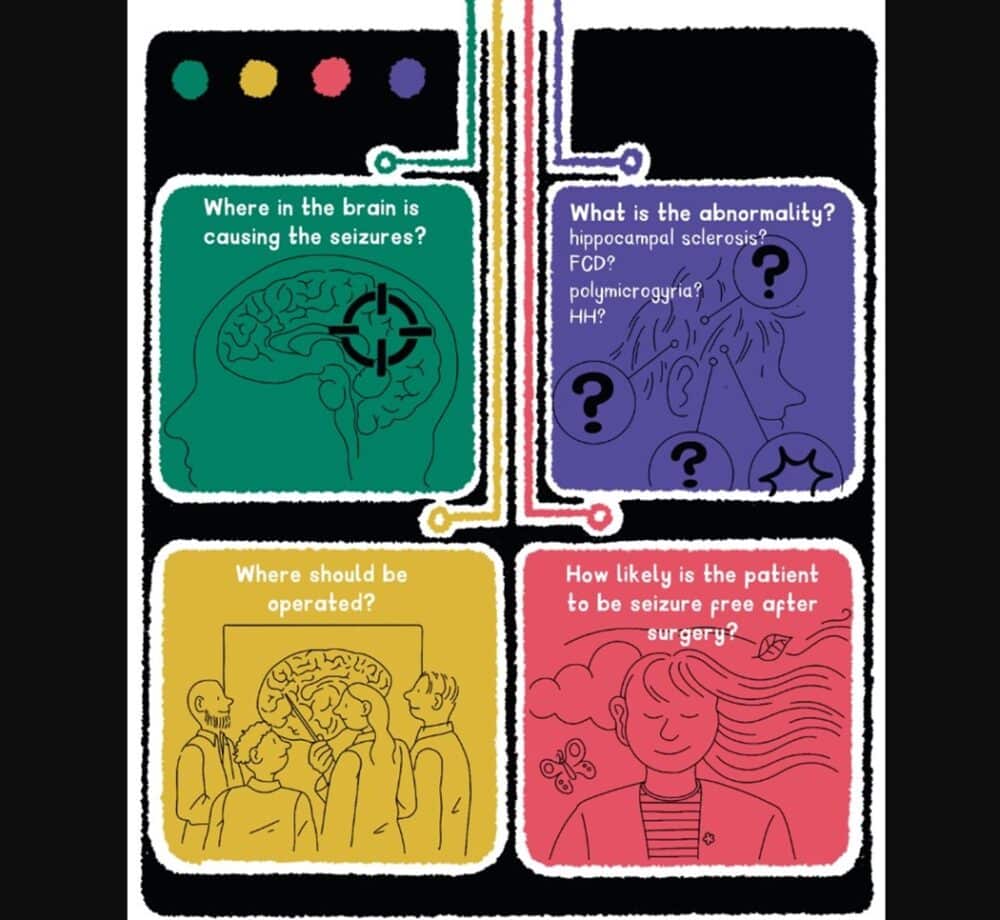
The standard treatment in these drug-resistant cases is the surgical removal of the lesion. This intervention alone manages to cure the condition and improves the patient’s cognitive development in the case of the patient being a child. However, identifying these abnormalities with MRI imaging is an ongoing challenge for clinicians, as sometimes drug-resistant epilepsy patients can have normal-looking scans, due to either the very subtle character of their brain abnormalities or even because of problems such as movement during the exam, for example.
Using AI
That is why a research group led by Dr. Sophie Adler-Wagstyl, Academic Clinical Fellow of the UCL (University College of London) Great Ormond Street Institute of Child Health, decided to investigate if an artificial intelligence (AI) algorithm could assist identification of even very subtle cases of FCD.
To develop a reliable AI algorithm, one needs to train it using examples from a wide variety of patients; a massive amount of data which is known in medical practice as “real-world evidence” (RWE).
As individual epilepsy centers typically treat only a small number of patients with this abnormality annually, the group decided to create the Multi-centre Epilepsy Lesion Detection (MELD) Project to collate 1,015 MRI scans (both patients and controls) from 22 centers across the world.
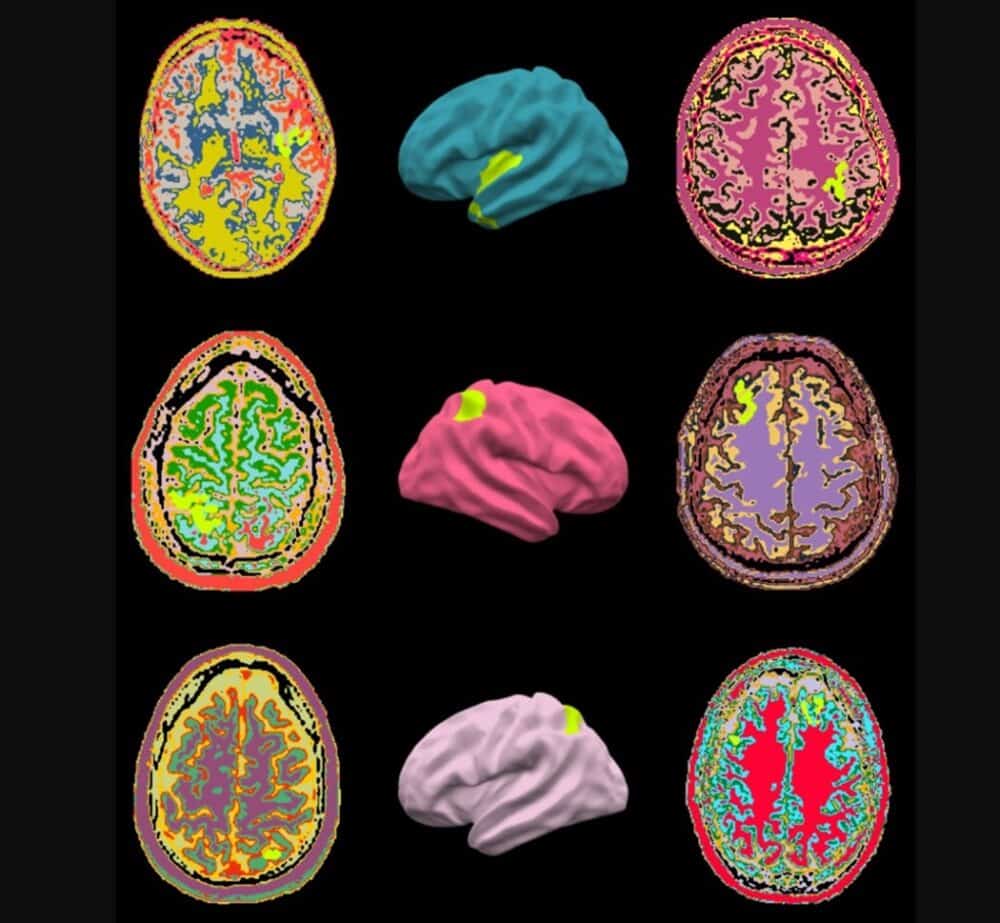
The scientists then analyzed features from all these MRI scans—such as how thick or folded the brain surface was—and measured them at around 300,000 locations in each subject’s brain. Expert radiologists from their team then labeled areas on the MRI scans as either being healthy or abnormal, and that enabled the team to train the algorithm to recognize patterns of features that characterize this particular FCD brain abnormality.
This bank of FCD data being used by the MELD Project is currently the largest of its kind in the whole world.
The MELD Project
The results of MELD Project’s research have been published in the journal Brain during the second half of 2022. Overall, the algorithm was able to detect these abnormalities in 67% of patients. A third of this group had previously had their MRI scans reported as normal—meaning that lesions, particularly challenging to identify by eye, were missed.
There is, however, room for improvement. AI algorithms commonly work as “black boxes”: they learn patterns from data rather than being explicitly programmed to make decisions. Consequently, it can sometimes be difficult to understand the logic behind a decision made by the AI.
So, the MELD Project added additional features so that the AI conclusions could be more easily understood by calculating which features contributed most to the final prediction. In other words, the information used by the algorithm to reach its conclusion is summarized into a supplementary report highlighting where and why in the brain the AI detected the abnormalities.
In addition to more precise diagnoses, the accurate identification of a lesion’s size and location is particularly important in cases of surgical removal. And finally, introducing ways to harmonize the data was another necessary challenge.
(Credit: MELD Project)
Konrad Wagstyl, one of the scientists of the MELD Project, told MedicalExpo e-Magazine:
“Typically, AI algorithms don’t do very well learning (distinguishing) from different types of scanners, countries, age groups. So, we introduced a number of methods to account for these sources of variability.”
It is important to remember though that no AI algorithm is perfect. Despite ever continuing advances, incorporating this type of technology into clinical practice requires certain precautions.
For instance, there is always the possibility that the MELD Project’s algorithm’s findings reflect MRI artifacts problems, such as patient movement or low image quality rather than true brain abnormalities. That is one more reason why the AI reports—just as with any traditional exam results—need to be analyzed alongside other investigations when surgery for epilepsy surgery is being planned.
At least 65 epilepsy surgery centers are already using the MELD algorithm. Meanwhile, the group continues to work to make the algorithm more powerful by collecting increased data from cases of epilepsy caused by other problems. Konrad explained:
“Focal epilepsy can be caused by a number of abnormalities beyond FCD. So, we have started a new MELD focal epilepsy project putting together a larger dataset, from more countries around the world, to make sure our tools work for this broad range of people, places and pathologies.”